City Footcare NYC
Surgery & Medicine of the Foot & Ankle
End Foot Pain Now
Welcome to CityFootcare.com!
We are group of 4 podiatrists located in Midtown Manhattan.
We offer the best care in Podiatric Medicine and Surgery in NYC.
The doctors at City Footcare NYC are the most compassionate and skilled foot doctors in the New York City Metro area and the country. Our office is conveniently located in Midtown Manhattan near Grand Central Station. We take great pride in providing excellent medical care along with great bedside manner and take the extra time to explain your problems and the treatment options in detail.
At City Footcare NYC we treat all problems related to the foot and ankle. We use state of the art diagnostic and therapeutic equipment. When your problem requires surgery, you can rest assured that you are in the hands of a competent and highly trained surgeon. Most of our doctors perform surgery and Dr. Sergi specifically only does foot surgery and not general podiatry (ask about individual providers).
Dr. Sergi has been called the best foot surgeon in NYC and the best bunion surgeon in NYC. The doctor performs all foot and ankle surgery including traditional open surgery, minimally invasive surgery, laser surgery, radio frequency surgery and extra-corporeal shock wave therapy. He is surgery center affiliated.
To resolve all of your foot and ankle problems, simply look around this site and make an appointment with the doctors at City Footcare NYC today. Your feet will be glad you did!
SLIMLINE BUNIONECTOMY: Precision bunion correction with a slim, tissue‑respecting approach
The Slimline Bunionectomy is a refined method Dr. Emanuel Sergi uses to realign the big toe, relieve pain, and improve function—while keeping soft‑tissue disruption to a minimum. This page summarizes the technique, candidacy, recovery, and how to get started at City Footcare in New York City.

End foot pain now!
You don’t have to spend another day suffering from foot pain! Let the City Footcare NYC doctors help you to END FOOT PAIN NOW! Call today to schedule an appointment and take the first step toward many more comfortable steps in the future.

Compassionate and caring
- Full treatment Facility
- Latest technology
- Most Insurances Accepted
- Convenient Location
Office Hours
A fun cartoon to explain bunion surgery!

Experts in Foot Surgery
When your problem requires surgery, you can rest assured that you are in the hands of a competent and highly trained surgeon.
Dr. Sergi and the City Footcare NYC Doctors have been called the best foot surgeons in NYC and the best bunion surgeons in NYC.
The doctors perform all foot and ankle surgery including traditional open surgery, minimally invasive surgery, laser surgery, radio frequency surgery and extra-corporeal shock wave therapy.
Dr. Sergi and the City Footcare NYC Doctors are experts in all aspects of foot surgery. They are very detail oriented from start to finish.
A good surgical outcome starts prior to entering the operating room. After expertly diagnosing patients’ conditions, they plan out the procedures with great skill.
In the operating room they are skillful and precise. They also take into consideration aesthetics with incision planning and plastic surgery type suturing techniques.
They are surgery center credentialled & affiliated.
Please see the medical DISCLAIMER on the 'about this blog page'.
Our Google Reviews.
"Dr. Sergi is knowledgeable and has good experience of fixing foot problem. He explains clearly the operation procedure and post-op care. He has confidence in his operation. He is also considerate of patient and has a warm heart to wrap surgical foot with bright color bandage. This is my third week since my surgery and I feel good to see my foot is free of bunion. I don't have pain from bunion or surgery. I am very lucky my foot has been fixed by a successful doctor who is expert in foot care operation."
"The best decision I could of done was to do my foot surgery with Dr. Emanuel Sergi.
He is the best, very caring and very professional.
I went to him for a second opinion and I am so glad I decided to do my foot surgery with him.
All I had to do was follow his instructions and my foot feels good and it’s healing very good also.
Thank you Dr. Sergi."
Recent blog posts are below:
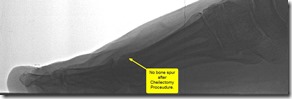
Heel Pain No More: Why Calcaneus Spur Surgery is the Best Option
Calcaneus Spur Removal Surgery
Heel pain is a debilitating condition that can disrupt daily activities and limit mobility. One of the most common causes of chronic heel pain is a calcaneus spur, also known as a heel spur. This bony growth on the underside of the heel can cause significant discomfort, particularly during walking or standing for extended periods. For many patients, conservative treatments such as rest, physical therapy, and orthotics may not provide adequate relief. In these cases, calcaneus spur surgery can be a highly effective solution. This blog will explore why calcaneus spur surgery might be the best option for those suffering from persistent heel pain and how it can improve your quality of life.
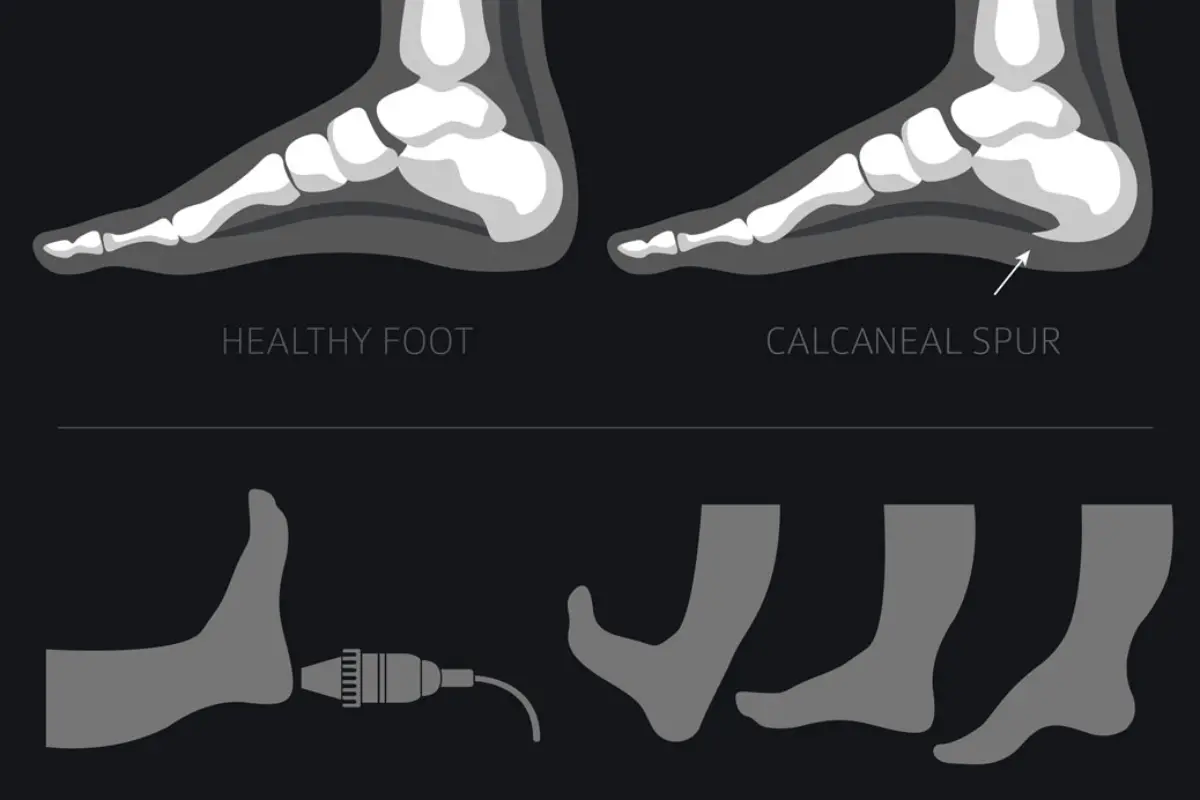
Understanding Calcaneus Spurs and Their Impact
A calcaneus spur, or heel spur, is a bony outgrowth that forms on the heel bone (calcaneus). These spurs develop over time due to repetitive stress on the heel, often associated with plantar fasciitis, flat feet, or high arches. Heel spurs can also result from the natural aging process, poor footwear choices, or overuse in activities like running, walking, or standing on hard surfaces.
Heel spurs themselves are not always painful, but they can irritate the surrounding soft tissues, leading to inflammation, pain, and swelling. The discomfort is usually felt in the bottom of the heel and may worsen with activity, especially after long periods of rest, such as the first steps in the morning. Left untreated, calcaneus spurs can make walking and standing unbearable, severely impacting one’s mobility and overall quality of life.
When Conservative Treatments Fall Short
For many individuals suffering from heel pain caused by calcaneus spurs, conservative treatments are often the first line of defense. These non-surgical treatments may include:
- Rest and activity modification
- Stretching exercises and physical therapy
- Custom orthotics to provide better foot support
- Anti-inflammatory medications to reduce swelling and pain
- Corticosteroid injections to reduce inflammation
While these treatments can provide temporary relief, they may not fully address the underlying issue. Patients with chronic or severe heel pain may find that these methods fail to deliver long-term results. In such cases, surgery may be the next best step to eliminate the source of the problem and restore full function to the foot.
What is Calcaneus Spur Surgery?
Calcaneus spur surgery is a minimally invasive procedure that involves removing the bony growth from the heel bone to alleviate pain and restore mobility. During the surgery, the podiatrist makes a small incision near the heel and carefully removes the spur. The surrounding tissue may also be examined to ensure that any inflammation or damage is properly addressed. The procedure is typically performed under local anesthesia, and patients can often return home the same day.
Calcaneus spur surgery not only removes the painful spur but also addresses any damage to the surrounding plantar fascia, which is often a contributing factor to the pain. The goal of the surgery is to provide long-lasting relief and allow the patient to return to their regular activities without the constant burden of heel pain.
Benefits of Calcaneus Spur Surgery
One of the primary benefits of calcaneus spur surgery is the long-term relief from heel pain. By removing the bony growth, the source of irritation is eliminated, allowing the foot to heal properly. Many patients experience a significant reduction in pain within a few weeks of the surgery and are able to resume normal activities shortly thereafter.
Another major benefit is the minimally invasive nature of the procedure. With modern surgical techniques, the incision is small, resulting in less tissue damage, minimal scarring, and a quicker recovery time compared to more invasive foot surgeries. Patients often experience less postoperative pain and swelling, which allows them to get back on their feet faster.
For those who have struggled with heel pain for months or even years, calcaneus spur surgery can be life-changing. The ability to walk, stand, and engage in physical activities without discomfort can greatly enhance one’s overall quality of life.
The Recovery Process
Recovery from calcaneus spur surgery is typically straightforward, though it does require patience and adherence to postoperative care instructions. After the surgery, patients may need to wear a protective boot or cast to immobilize the foot and allow the incision to heal. It is important to avoid putting weight on the foot during the initial recovery phase to prevent complications.
Most patients can begin walking with the help of crutches within a few days of the surgery. Physical therapy may be recommended to help restore strength, flexibility, and range of motion to the foot. The full recovery process usually takes several weeks, but many patients notice a dramatic improvement in pain relief soon after the procedure.
Following calcaneus spur surgery, it is important to follow a podiatrist’s advice on proper footwear and foot care to prevent the recurrence of heel pain. Supportive shoes, custom orthotics, and regular stretching exercises can help maintain the benefits of the surgery and reduce the risk of developing future foot issues.
Patient Success Story: Michael’s Path to Pain-Free Living
Michael, a 45-year-old avid runner, had been suffering from chronic heel pain for over two years. Despite trying various conservative treatments like physical therapy and orthotics, the pain persisted, making it difficult for him to continue his running routine. Frustrated with the lack of progress, Michael decided to visit Citi Footcare for a consultation with Dr. Emanuel Sergi.
After a thorough evaluation, Dr. Sergi diagnosed Michael with a calcaneus spur and recommended surgery as the best option to eliminate his pain. The procedure was performed successfully, and within a few weeks, Michael was back on his feet. The surgery not only relieved his heel pain but also allowed him to return to running without discomfort. Michael’s experience highlights the effectiveness of calcaneus spur surgery and the exceptional care provided by Dr. Sergi and the team at Citi Footcare.
Why Citi Footcare is the Best Choice for Calcaneus Spur Surgery in New York City
When it comes to calcaneus spur surgery, choosing the right podiatrist is crucial for achieving the best possible outcomes. Citi Footcare, led by Dr. Emanuel Sergi, is recognized as one of the leading podiatry practices in New York City. Dr. Sergi is a highly skilled podiatrist with extensive experience in both conservative and surgical treatments for foot and ankle conditions.
At Citi Footcare, patients receive personalized treatment plans tailored to their unique needs. Dr. Sergi and his team are committed to providing state-of-the-art care using the latest minimally invasive techniques. From the initial consultation to post-surgical follow-ups, patients can expect comprehensive care that focuses on long-term relief and improved foot health.
Located in the heart of New York City, Citi Footcare is easily accessible and offers convenient scheduling for patients seeking expert foot care. With a track record of successful surgeries and satisfied patients, Citi Footcare is the trusted choice for calcaneus spur surgery in NYC.
Patient Success Story: Lloyd’s Journey to Pain-Free Living
Lloyd, a 52-year-old accountant in New York City, had always been on his feet, moving around the bustling city. However, he began experiencing severe heel pain that gradually worsened over the years. The pain, especially sharp in the mornings and after long days of standing, started to limit his mobility. After trying various treatments like orthotics and pain relievers, Lloyd’s discomfort persisted, and he found it difficult to keep up with his active lifestyle. Frustrated, Lloyd decided to seek professional help and visited Citi Footcare.
During his consultation, Dr. Emanuel Sergi quickly diagnosed Lloyd with a calcaneus spur. After explaining the treatment options, Dr. Sergi recommended surgery to remove the bony growth and restore Lloyd’s mobility. Nervous but optimistic, Lloyd agreed to proceed with the minimally invasive calcaneus spur surgery.
The procedure was a success. Dr. Sergi skillfully removed the heel spur, and Lloyd was able to walk with minimal discomfort the very next day. Within a few weeks, Lloyd noticed a dramatic reduction in pain and began to enjoy his daily walks around the city again. Thanks to the expert care at Citi Footcare, Lloyd was able to reclaim his active lifestyle, free from the debilitating heel pain that had plagued him for years. His story highlights the life-changing benefits of calcaneus spur surgery and the exceptional care provided by Dr. Sergi and his team.
Take the Next Step with Citi Footcare
If you are suffering from persistent heel pain caused by a calcaneus spur, consider the benefits of calcaneus spur surgery at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved mobility through advanced surgical techniques. Schedule a consultation today to learn more about how calcaneus spur surgery can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare
122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
Revolutionizing Plantar Fasciitis treatment: The Tenex Advantage
Tenex Procedure for Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain, affecting millions of people each year. This condition occurs when the thick band of tissue that runs across the bottom of the foot, known as the plantar fascia, becomes inflamed. The result is often sharp, stabbing pain in the heel, particularly during the first steps of the day. While there are many treatments available, ranging from physical therapy to injections, one procedure is revolutionizing the way plantar fasciitis is treated: the Tenex procedure. In this blog, we explore how the Tenex procedure offers significant advantages over traditional treatments and why it might be the best option for those suffering from chronic heel pain.
Understanding Plantar Fasciitis
Plantar fasciitis develops when the plantar fascia, a ligament that supports the arch of the foot, experiences repeated stress and strain. This condition is common among runners, athletes, and individuals who spend a lot of time on their feet. Over time, small tears can develop in the fascia, leading to inflammation and pain. The pain is typically worse in the morning or after periods of inactivity, as the fascia tightens during rest and is suddenly stretched when walking resumes.
Plantar fasciitis can be debilitating, affecting an individual’s ability to walk, work, and engage in physical activities. Traditional treatments include rest, ice, physical therapy, orthotics, anti-inflammatory medications, and corticosteroid injections. While these treatments can be effective for some patients, others find that their symptoms persist despite these efforts. For those with chronic or severe plantar fasciitis, surgical intervention was often considered the next step. However, surgery comes with its own risks and lengthy recovery times, making it a less desirable option for many.
The Tenex Procedure: A Minimally Invasive Solution
The Tenex procedure represents a significant advancement in the treatment of plantar fasciitis. This minimally invasive technique is designed to remove the damaged tissue that is causing pain while leaving the healthy tissue intact. The procedure is performed using a specialized device that emits ultrasonic energy to break down and remove the diseased tissue through a small incision.
The Tenex procedure is performed under local anesthesia and typically takes less than 30 minutes to complete. Because the procedure is minimally invasive, it results in less pain, a lower risk of complications, and a faster recovery time compared to traditional surgery. Patients are usually able to walk immediately after the procedure and can return to their normal activities within a few weeks.
Benefits of the Tenex Procedure
One of the primary benefits of the Tenex procedure is the rapid relief of pain. Many patients report significant improvement in their symptoms within days of the procedure. Because the Tenex device precisely targets and removes the damaged tissue, the source of the pain is effectively eliminated, allowing the plantar fascia to heal properly.
Another advantage is the minimally invasive nature of the procedure. Unlike traditional surgery, which requires large incisions and extensive downtime, the Tenex procedure involves only a tiny incision, resulting in minimal scarring and a much quicker recovery. Patients who undergo the Tenex procedure can often return to work and their daily activities much sooner than those who undergo traditional surgery.
Additionally, the Tenex procedure has a lower risk of complications compared to more invasive surgical options. The precision of the ultrasonic device allows for targeted treatment, reducing the likelihood of damage to surrounding healthy tissue. This targeted approach also minimizes the risk of infection and other postoperative complications, making it a safer option for many patients.
Improved Quality of Life
For many patients, the decision to undergo the Tenex procedure is driven by the desire to improve their quality of life. Chronic heel pain can significantly impact daily activities, making it difficult to walk, stand, or engage in physical exercise. The Tenex procedure offers a solution that not only alleviates pain but also allows patients to regain their mobility and return to the activities they enjoy.
Patients who have undergone the Tenex procedure often report a marked improvement in their overall quality of life. The ability to walk without pain, participate in sports, and enjoy an active lifestyle can have a profound impact on both physical and mental well-being. For those who have struggled with plantar fasciitis for years, the Tenex procedure offers a chance to reclaim their life from chronic pain.
Advances in Technology and Technique
The success of the Tenex procedure is largely due to the advancements in technology and surgical techniques. The development of the Tenex device, which uses ultrasonic energy to precisely remove damaged tissue, represents a major breakthrough in the treatment of plantar fasciitis. This technology allows for a level of precision and control that was previously unattainable with traditional surgical methods.
The technique used in the Tenex procedure also reflects a shift towards less invasive treatments in the medical field. By minimizing the trauma to the body, patients can experience faster healing times, less pain, and a quicker return to normal activities. These advancements have made the Tenex procedure an attractive option for patients seeking an effective and minimally invasive solution to chronic heel pain.
Patient Success Story: Maria’s Experience with Tenex
Sophia, a young professional in New York City, had struggled with painful corns for years. The discomfort affected her ability to wear her favorite shoes and limited her participation in social and physical activities. After trying various over-the-counter treatments without success, Sophia decided to seek help from Citi Footcare.
During her consultation with Dr. Emanuel Sergi, Sophia learned about the cosmetic corn removal procedure and how it could help her regain her confidence and comfort. The procedure was a success, and within weeks, Sophia noticed a significant improvement in both the appearance and feel of her feet. The pain was gone, and she could finally wear the shoes she loved without discomfort. Sophia’s positive experience highlights the transformative potential of cosmetic corn removal and the exceptional care provided by Dr. Sergi and his team.
Why Citi Footcare is the Best Choice for the Tenex Procedure in New York City
Choosing the right podiatrist for the Tenex procedure is crucial for achieving the best possible outcomes. Citi Footcare, led by Dr. Emanuel Sergi, stands out as the premier choice for several reasons. Dr. Sergi and his team have extensive experience in performing the Tenex procedure and are dedicated to providing personalized care tailored to each patient’s unique needs.
Citi Footcare is committed to staying at the forefront of medical advancements, utilizing the latest technology and techniques to ensure optimal results. The practice’s patient-centered approach focuses on comprehensive care, from the initial consultation to post-procedure follow-up. Located conveniently in the heart of New York City, Citi Footcare offers easy access to top-tier podiatric care, making it the ideal choice for patients seeking relief from plantar fasciitis.
Patient Success Story: Kristina’s Return to Pain-Free Living
Kristina, a dedicated teacher and avid walker, had always enjoyed her daily strolls through Central Park. However, persistent heel pain began to interfere with her routine, turning her once-enjoyable walks into painful ordeals. The pain, which was especially intense in the mornings, gradually became so severe that it affected her ability to stand and teach comfortably. After trying various conservative treatments without success, Kristina knew she needed a more effective solution and sought help from Citi Footcare.
During her consultation with Dr. Emanuel Sergi, Kristina learned that she was suffering from chronic plantar fasciitis. Dr. Sergi recommended the Tenex procedure, a minimally invasive treatment designed to target and remove the damaged tissue causing her pain. Intrigued by the prospect of a quick recovery and lasting relief, Kristina decided to proceed with the procedure.
The Tenex procedure was performed with precision, and Kristina was amazed at how quick and straightforward it was. She was able to walk out of the clinic the same day, feeling optimistic about her recovery. Within just a few weeks, Kristina noticed a dramatic reduction in her heel pain. The once-dreaded first steps of the morning were now pain-free, and she gradually returned to her cherished walks in the park. Thanks to the Tenex procedure and the exceptional care she received at Citi Footcare, Kristina was able to reclaim her active lifestyle and continue doing what she loved most without discomfort.
Take the Next Step with Citi Footcare
If you are suffering from chronic heel pain due to plantar fasciitis, the Tenex procedure at Citi Footcare could be the solution you have been searching for. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved foot function through advanced treatments like the Tenex procedure. Schedule a consultation today to learn more about how the Tenex procedure can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
Say Goodbye to Painful Corns: The Art of Cosmetic Corn Removal
Mastering the Art of Cosmetic Corn Removal
Corns are a common foot ailment that can cause significant discomfort and affect the appearance of the feet. These hardened areas of skin typically develop due to repeated friction and pressure, often from ill-fitting shoes or abnormal foot structure. While corns can be unsightly and painful, many individuals endure them, not knowing that an effective, cosmetic solution exists. This blog delves into the art of cosmetic corn removal, highlighting why it might be the best option for those looking to restore comfort and aesthetics to their feet.
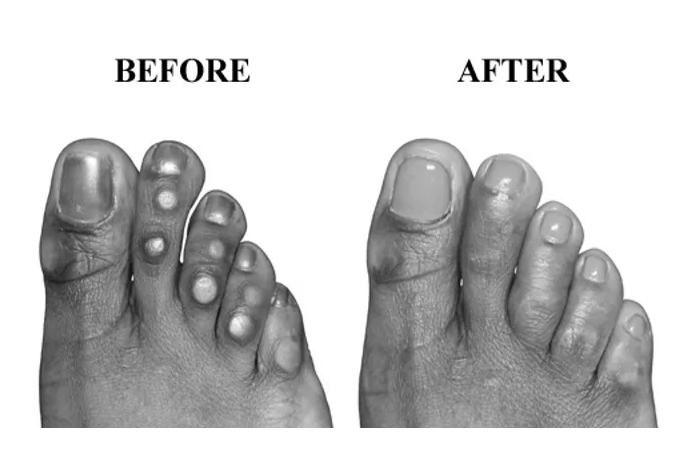
Understanding Corns and Their Impact
Corns are thickened layers of skin that form in response to friction and pressure. They commonly appear on the tops, sides, and tips of the toes or on the balls of the feet. Corns are often mistaken for calluses, but they differ in that corns are usually smaller, more localized, and can be more painful due to the deeper layers of skin they affect.
The pain from corns can be debilitating, making it difficult to walk or wear certain types of shoes. Over time, the discomfort can lead to a reduction in physical activity and a decrease in overall quality of life. Additionally, corns can be a cosmetic concern, causing embarrassment and self-consciousness, particularly in social settings where bare feet or open-toed shoes are involved.
What is Cosmetic Corn Removal?
Cosmetic corn removal, also known as arthroplasty with medial incision, is a surgical procedure designed to remove corns while addressing the underlying causes that lead to their formation. Unlike over-the-counter treatments that simply reduce the appearance of corns temporarily, cosmetic corn removal offers a permanent solution by correcting the foot’s structure and eliminating the source of friction and pressure.
The procedure involves making a small incision near the corn to access and remove the hardened skin and any underlying bone that may be contributing to the problem. The incision is strategically placed to minimize visible scarring and to ensure that the foot’s natural contours are preserved. This approach not only alleviates pain but also enhances the foot’s appearance, making it an ideal option for those seeking both functional and cosmetic improvement.
Benefits of Cosmetic Corn Removal
One of the primary benefits of cosmetic corn removal is the relief from pain and discomfort. By removing the corn and correcting the underlying bone structure, patients can walk and wear shoes without the constant irritation that corns cause. This procedure can significantly improve mobility and allow individuals to return to their normal activities with greater comfort.
Another major advantage is the cosmetic improvement. Corns can be unsightly, and their removal can greatly enhance the appearance of the feet. The minimal incision used in the procedure ensures that scarring is minimal, allowing patients to enjoy smooth, blemish-free skin. This is particularly important for those who are self-conscious about their feet and want to feel confident in their appearance.
Improved Quality of Life
For many patients, the decision to undergo cosmetic corn removal is driven by the desire to improve their quality of life. The ability to walk, run, and engage in physical activities without pain is a significant benefit of this procedure. Patients who have undergone cosmetic corn removal often report higher satisfaction levels due to the improved function and appearance of their feet.
The minimally invasive nature of the surgery also means that patients can enjoy a more comfortable recovery period. With less postoperative pain and swelling, individuals can return to work and their daily routines more quickly. This contributes to a better overall experience and a faster return to normal life.
Advances in Surgical Techniques
The success of cosmetic corn removal is largely due to advancements in surgical techniques and technology. Surgeons now have access to high-precision instruments and imaging tools that allow for better visualization and accuracy during the procedure. These innovations have made it possible to perform the surgery with a high degree of precision, leading to better outcomes and fewer complications.
Modern fixation devices, such as screws and plates, provide enhanced stability during the healing process. These devices ensure that the bones remain in the correct alignment, reducing the risk of recurrence and promoting optimal healing. The use of these advanced tools and techniques has revolutionized corn removal surgery, offering patients more effective and reliable treatment options.
The Recovery Process
Recovery from cosmetic corn removal involves a period of rest and rehabilitation. Initially, the foot is typically placed in a protective dressing or bandage to protect the surgical site and allow for proper healing. Patients are advised to keep weight off the affected foot and use crutches to aid in mobility.
Physical therapy may be recommended to help restore strength, flexibility, and range of motion. The duration of the recovery period varies depending on the severity of the corn and the individual’s overall health, but most patients can expect to return to normal activities within a few weeks. Adhering to postoperative care instructions is crucial to ensure successful healing and prevent complications.
Patient Success Story: Sophia’s Journey to Beautiful Feet
Sophia, a young professional in New York City, had struggled with painful corns for years. The discomfort affected her ability to wear her favorite shoes and limited her participation in social and physical activities. After trying various over-the-counter treatments without success, Sophia decided to seek help from Citi Footcare.
During her consultation with Dr. Emanuel Sergi, Sophia learned about the cosmetic corn removal procedure and how it could help her regain her confidence and comfort. The procedure was a success, and within weeks, Sophia noticed a significant improvement in both the appearance and feel of her feet. The pain was gone, and she could finally wear the shoes she loved without discomfort. Sophia’s positive experience highlights the transformative potential of cosmetic corn removal and the exceptional care provided by Dr. Sergi and his team.
Why Citi Footcare is the Best Choice for Cosmetic Corn Removal in New York City
Choosing the right podiatrist for cosmetic corn removal is crucial for achieving the best possible outcomes. Citi Footcare stands out as the premier choice for several reasons. The team at Citi Footcare, led by Dr. Emanuel Sergi, consists of highly experienced and skilled podiatrists who specialize in minimally invasive foot surgeries. They utilize the latest technology and surgical techniques to provide top-notch care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a proven track record of successful surgeries and satisfied patients who have experienced significant improvements in their quality of life. Located conveniently in the heart of New York City, Citi Footcare offers easy access to top-tier podiatric care.
Patient Success Story: Danny’s Journey to Pain-Free Feet
Danny, an active professional who loved staying on his feet, found himself increasingly troubled by painful corns that made even the simplest tasks unbearable. The constant discomfort affected his ability to walk comfortably and forced him to avoid wearing his favorite shoes. Frustrated and self-conscious about the appearance of his feet, Danny decided it was time to seek professional help. That’s when he turned to Citi Footcare and Dr. Emanuel Sergi.
During his consultation, Dr. Sergi thoroughly assessed Danny’s condition and explained how cosmetic corn removal could provide both relief from pain and a significant cosmetic improvement. Danny felt reassured by Dr. Sergi’s expertise and the detailed explanation of the procedure. Confident that he was in the best hands, Danny decided to proceed with the surgery.
The procedure was a resounding success. Dr. Sergi skillfully removed the painful corns and addressed the underlying structural issues, ensuring that Danny’s feet would heal properly without the risk of the corns returning. The minimally invasive nature of the surgery meant that Danny experienced minimal discomfort during his recovery. Within a few weeks, Danny was not only walking pain-free but also proudly showing off his smooth, corn-free feet. The results exceeded his expectations, and he felt a renewed sense of confidence and comfort in his daily life.
Danny’s positive experience at Citi Footcare underscores the life-changing benefits of cosmetic corn removal. Thanks to Dr. Sergi and his team, Danny was able to reclaim his active lifestyle and enjoy the simple pleasures of walking without pain. His story is a testament to the transformative impact of expert podiatric care.
Take the Next Step with Citi Footcare
If you are struggling with painful or unsightly corns, consider cosmetic corn removal at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved foot appearance through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how cosmetic corn removal can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
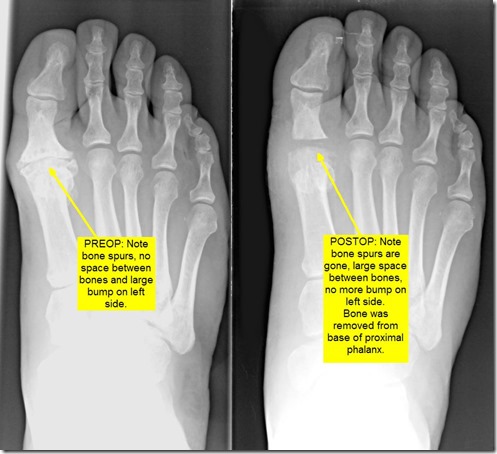
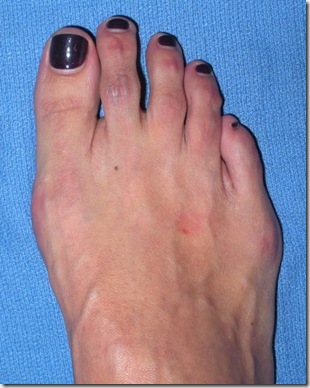
Sculpting Relief: Why Modified Scarf Bunionectomy Might Be Your Best Option
Sculpting Relief: Why Modified Scarf Bunionectomy Might Be Your Best Option
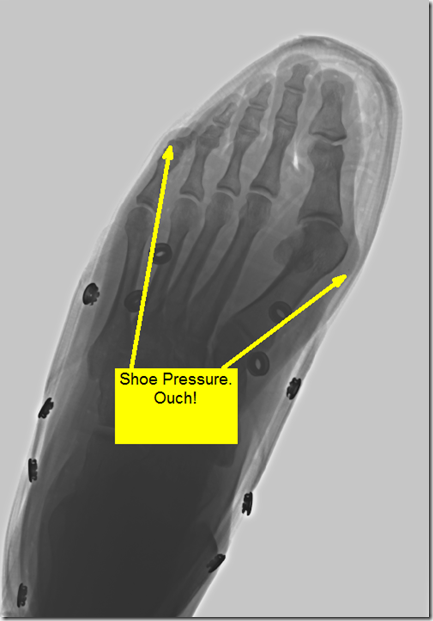
Bunions are a common foot deformity that can cause significant discomfort and affect daily activities. This painful bony bump forms at the joint where the big toe meets the foot, often leading to swelling, soreness, and restricted movement. While many treatment options exist, one of the most effective surgical solutions is the Modified Scarf Bunionectomy. This procedure is designed to alleviate pain, improve foot function, and enhance quality of life for those suffering from bunions.
Understanding Bunions and Their Impact
Bunions, medically known as hallux valgus, occur when the big toe deviates toward the other toes, causing a misalignment in the joint. This misalignment can lead to a prominent bump on the side of the foot. Factors contributing to bunion development include genetics, wearing tight or ill-fitting shoes, and conditions like arthritis. Bunions can lead to significant pain, inflammation, and difficulty finding comfortable footwear.
The impact of bunions extends beyond physical discomfort. Many individuals with bunions experience a decrease in their quality of life due to limited mobility and activity restrictions. This can lead to frustration and a desire for effective treatment options that offer long-lasting relief.
What is a Modified Scarf Bunionectomy?
The Modified Scarf Bunionectomy is a surgical procedure designed to correct the alignment of the first metatarsal bone and the big toe joint. This procedure involves making a Z-shaped cut in the metatarsal bone, allowing the surgeon to reposition and stabilize the bone in a more natural alignment. The bone is then secured using screws or other fixation devices to ensure proper healing.
This technique offers several advantages over traditional bunionectomy procedures. The Modified Scarf Bunionectomy provides enhanced stability and precise control over the bone’s realignment, leading to better long-term outcomes and reduced risk of recurrence. The procedure is known for its versatility, as it can address a wide range of bunion deformities, from mild to severe.
Benefits of Modified Scarf Bunionectomy
One of the primary benefits of the Modified Scarf Bunionectomy is the significant improvement in foot alignment and function. By addressing the underlying cause of the bunion deformity, this procedure provides long-lasting relief from pain and discomfort. Patients who undergo the Modified Scarf Bunionectomy often experience a marked reduction in pain and swelling, allowing them to resume their daily activities without limitation.
Another key advantage of this procedure is the minimally invasive nature of the surgery. Modern surgical techniques allow for smaller incisions, resulting in less tissue damage and faster recovery times. Patients typically experience less postoperative pain and can return to their normal activities sooner than with traditional bunion surgery.
Improved Quality of Life
For many patients, the decision to undergo a Modified Scarf Bunionectomy is driven by the desire to improve their quality of life. The ability to walk, run, and engage in physical activities without pain is a significant benefit of this procedure. Patients who have undergone the Modified Scarf Bunionectomy often report higher satisfaction levels due to the improved function and appearance of their feet.
The minimally invasive nature of the surgery also means that patients can enjoy a more comfortable recovery period. With less postoperative pain and swelling, individuals can return to work and their daily routines more quickly. This contributes to a better overall experience and a faster return to normal life.
Advances in Surgical Techniques
The success of the Modified Scarf Bunionectomy is largely due to advancements in surgical techniques and technology. Surgeons now have access to high-precision instruments and imaging tools that allow for better visualization and accuracy during the procedure. These innovations have made it possible to perform the surgery with a high degree of precision, leading to better outcomes and fewer complications.
Modern fixation devices, such as screws and plates, provide enhanced stability during the healing process. These devices ensure that the bones remain in the correct alignment, reducing the risk of recurrence and promoting optimal healing. The use of these advanced tools and techniques has revolutionized bunion surgery, offering patients more effective and reliable treatment options.
The Recovery Process
Recovery from a Modified Scarf Bunionectomy involves a period of rest and rehabilitation. Initially, the foot is typically placed in a cast or boot to protect the surgical site and allow for proper healing. Patients are advised to keep weight off the affected foot and use crutches to aid in mobility.
Physical therapy is often recommended to help restore strength, flexibility, and range of motion. The duration of the recovery period varies depending on the severity of the bunion and the individual’s overall health, but most patients can expect to return to normal activities within a few months. Adhering to postoperative care instructions is crucial to ensure successful healing and prevent complications.
Rachel, a busy professional in New York City, had been struggling with bunion pain for years. The discomfort affected her ability to walk comfortably and limited her participation in social and physical activities. After consulting with Dr. Emanuel Sergi at Citi Footcare, Rachel learned about the Modified Scarf Bunionectomy and how it could help her regain her mobility and quality of life.
Rachel underwent the surgery and was amazed by the results. The procedure corrected the alignment of her big toe, and the pain and swelling subsided significantly. Within weeks, she was able to walk without discomfort and resume her active lifestyle. Rachel’s positive experience highlights the transformative potential of the Modified Scarf Bunionectomy and the exceptional care provided by Dr. Sergi and his team.
Patient Success Story: Rachel’s Journey
Rachel, a busy professional in New York City, had been struggling with bunion pain for years. The discomfort affected her ability to walk comfortably and limited her participation in social and physical activities. After consulting with Dr. Emanuel Sergi at Citi Footcare, Rachel learned about the Modified Scarf Bunionectomy and how it could help her regain her mobility and quality of life.
Rachel underwent the surgery and was amazed by the results. The procedure corrected the alignment of her big toe, and the pain and swelling subsided significantly. Within weeks, she was able to walk without discomfort and resume her active lifestyle. Rachel’s positive experience highlights the transformative potential of the Modified Scarf Bunionectomy and the exceptional care provided by Dr. Sergi and his team.
Why Citi Footcare is the Best Choice for Modified Scarf Bunionectomy in New York City
Choosing the right podiatrist for a Modified Scarf Bunionectomy is crucial for achieving the best possible outcomes. Citi Footcare stands out as the premier choice for several reasons. The team at Citi Footcare, led by Dr. Emanuel Sergi, consists of highly experienced and skilled podiatrists who specialize in minimally invasive foot surgeries. They utilize the latest technology and surgical techniques to provide top-notch care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a proven track record of successful surgeries and satisfied patients who have experienced significant improvements in their quality of life. Located conveniently in the heart of New York City, Citi Footcare offers easy access to top-tier podiatric care.
Patient Success Story: Rahman’s Journey to Pain-Free Living
Rahman, an avid hiker and nature enthusiast, had always enjoyed exploring the trails around New York. However, over the years, he began to experience severe pain and swelling in his big toe, making each hike increasingly unbearable. After trying various conservative treatments without success, Rahman decided to seek help from Citi Footcare.
During his consultation with Dr. Emanuel Sergi, Rahman learned that his bunion had progressed significantly and would require surgical intervention. Dr. Sergi recommended the Modified Scarf Bunionectomy, explaining how this procedure could correct the deformity and alleviate his pain. Feeling reassured by Dr. Sergi’s expertise and the comprehensive explanation of the procedure, Rahman decided to proceed with the surgery.
The surgery was a resounding success. Dr. Sergi skillfully realigned Rahman’s metatarsal bone, and the advanced fixation devices ensured proper healing. The minimally invasive nature of the Modified Scarf Bunionectomy meant that Rahman experienced less postoperative pain and a quicker recovery. With the support and guidance of the Citi Footcare team, Rahman followed his rehabilitation plan diligently, and within a few weeks, he was back on his feet.
Rahman’s positive experience at Citi Footcare transformed his life. The surgery not only relieved his pain but also restored his ability to enjoy hiking without discomfort. He was thrilled to return to the trails he loved, pain-free and with renewed confidence. Rahman’s story highlights the exceptional care and expertise of Dr. Emanuel Sergi and the Citi Footcare team, showcasing the life-changing impact of the Modified Scarf Bunionectomy.
Take the Next Step with Citi Footcare
If you are suffering from bunions and looking for a powerful and minimally invasive solution, consider the Modified Scarf Bunionectomy at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved foot function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how the Modified Scarf Bunionectomy can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare
122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800
The Breakthrough in Foot Health: Fifth Metatarsal Base Fracture Surgery Explained
The Breakthrough in Foot Health: Fifth Metatarsal Base Fracture Surgery Explained
The fifth metatarsal base fracture is a common injury, often resulting from twisting of the foot, overuse, or direct impact. This fracture, located at the base of the small toe’s metatarsal bone, can lead to significant pain and mobility issues. Addressing this injury effectively is crucial for restoring full function and preventing future complications. This blog delves into the intricacies of fifth metatarsal base fracture surgery, highlighting its benefits and why it might be the optimal solution for those suffering from this type of fracture.
Understanding Fifth Metatarsal Base Fractures
The fifth metatarsal base fracture is a common injury, often resulting from twisting of the foot, overuse, or direct impact. This fracture, located at the base of the small toe’s metatarsal bone, can lead to significant pain and mobility issues. Addressing this injury effectively is crucial for restoring full function and preventing future complications. This blog delves into the intricacies of fifth metatarsal base fracture surgery, highlighting its benefits and why it might be the optimal solution for those suffering from this type of fracture.
The Importance of Prompt and Proper Treatment
Timely intervention is crucial in managing fifth metatarsal base fractures. Delayed or inadequate treatment can result in improper healing, leading to chronic pain and instability. While non-surgical methods like rest, immobilization, and physical therapy can be effective for some fractures, others, particularly those that are displaced or involve the joint, may require surgical intervention to achieve optimal results.
What is Fifth Metatarsal Base Fracture Surgery?
Fifth metatarsal base fracture surgery involves realigning the broken bone fragments and securing them with surgical hardware such as screws, plates, or wires. This surgical procedure ensures that the bone heals correctly, restoring stability and function to the foot. The specific surgical approach depends on the type and severity of the fracture, as well as the patient’s overall health and activity level.
Benefits of Fifth Metatarsal Base Fracture Surgery
The primary benefit of fifth metatarsal base fracture surgery is the precise alignment and stabilization of the bone, which promotes proper healing. This surgical approach significantly reduces the risk of complications such as nonunion (failure of the bone to heal) or malunion (healing in an incorrect position), which can occur with non-surgical treatment.
Another major advantage is the restoration of foot function. Patients who undergo surgery typically experience a quicker and more complete recovery, allowing them to return to their normal activities, including sports and exercise, with reduced pain and improved stability. The surgical intervention also minimizes the likelihood of long-term complications such as arthritis or chronic pain.
Advances in Surgical Techniques
Advancements in surgical techniques and technology have made fifth metatarsal base fracture surgery more effective and less invasive. Minimally invasive procedures, improved fixation devices, and enhanced imaging techniques have all contributed to better outcomes for patients. These advancements have reduced recovery times, minimized complications, and improved overall patient satisfaction.
Surgeons now utilize high-precision instruments and imaging tools that allow for better visualization and accuracy during the procedure. These innovations have made it possible to perform the surgery with a high degree of precision, leading to better outcomes and fewer complications.
The Recovery Process
Recovery from fifth metatarsal base fracture surgery involves a period of immobilization followed by rehabilitation. Initially, the foot is typically placed in a cast or boot to protect the surgical site and allow for proper healing. Patients are advised to keep weight off the affected foot and use crutches to aid in mobility.
Physical therapy is often recommended to help restore strength, flexibility, and range of motion. The duration of the recovery period varies depending on the severity of the fracture and the individual’s overall health, but most patients can expect to return to normal activities within a few months. Adhering to postoperative care instructions is crucial to ensure successful healing and prevent complications.
Potential Risks and Considerations
As with any surgical procedure, there are potential risks associated with fifth metatarsal base fracture surgery. These can include infection, nerve damage, and complications related to anesthesia. However, these risks are relatively low, especially when the surgery is performed by an experienced podiatrist. Patients should discuss all potential risks and benefits with their surgeon to make an informed decision.
Long-Term Success and Follow-Up Care
The long-term success of fifth metatarsal base fracture surgery depends on several factors, including the surgeon’s expertise, the patient’s adherence to postoperative care instructions, and any underlying health conditions. Regular follow-up visits are crucial to monitor healing and address any concerns promptly. Most patients can expect significant pain relief and improved foot function that lasts for years.
Patient Success Story: David’s Journey to Recovery
David, an active athlete, suffered a fifth metatarsal base fracture while playing soccer. The pain and swelling were immediate, and he struggled to walk. After visiting Citi Footcare and consulting with Dr. Emanuel Sergi, David learned that his injury required surgical intervention for optimal healing. Dr. Sergi explained the procedure in detail, addressing all of David’s concerns and ensuring he felt comfortable with the decision.
The surgery was successful, and David followed his postoperative care plan meticulously. With the guidance of Dr. Sergi and the Citi Footcare team, David progressed through physical therapy and gradually regained strength and mobility in his foot. Within a few months, he was back on the soccer field, playing without pain or limitations. David’s positive experience underscores the effectiveness of fifth metatarsal base fracture surgery and the exceptional care provided by Citi Footcare.
Why Citi Footcare is the Best Choice for Fifth Metatarsal Base Fracture Surgery in New York City
Choosing the right podiatrist for fifth metatarsal base fracture surgery is crucial for achieving the best possible outcomes. Citi Footcare stands out as the premier choice for several reasons. The team at Citi Footcare, led by Dr. Emanuel Sergi, consists of highly experienced and skilled podiatrists who specialize in foot and ankle surgeries. They utilize the latest technology and surgical techniques to provide top-notch care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a proven track record of successful surgeries and satisfied patients who have experienced significant improvements in their quality of life. Located conveniently in the heart of New York City, Citi Footcare offers easy access to top-tier podiatric care.
Patient Success Story: Shaun’s Road to Recovery
Shaun, an avid runner and outdoor enthusiast, found his passion for fitness abruptly halted after a misstep during a trail run resulted in a painful fifth metatarsal base fracture. The injury left him unable to bear weight on his foot, and the prospect of long-term recovery loomed large. Seeking a solution that would get him back on his feet as quickly as possible, Shaun turned to Citi Footcare and the expertise of Dr. Emanuel Sergi.
During his consultation, Dr. Sergi thoroughly explained the nature of Shaun’s injury and the potential treatment options. Given the severity of the fracture and Shaun’s active lifestyle, Dr. Sergi recommended fifth metatarsal base fracture surgery. Shaun appreciated Dr. Sergi’s detailed explanation and reassurance about the procedure and recovery process. Feeling confident in the care he would receive, Shaun decided to proceed with the surgery.
The surgery was a success. Dr. Sergi skillfully realigned the fractured bone and secured it with precision, ensuring optimal healing. Shaun was provided with a comprehensive postoperative care plan that included rest, immobilization, and a tailored physical therapy regimen. The support and guidance from the Citi Footcare team were instrumental in Shaun’s recovery.
As weeks turned into months, Shaun experienced remarkable progress. The pain subsided, and he gradually regained strength and mobility in his foot. With dedication to his rehabilitation plan and regular follow-ups at Citi Footcare, Shaun was soon able to return to his beloved outdoor activities. The successful surgery and recovery not only restored Shaun’s physical capabilities but also reignited his passion for running. Shaun’s story is a testament to the exceptional care provided by Dr. Emanuel Sergi and the Citi Footcare team, showcasing the transformative impact of fifth metatarsal base fracture surgery.
Take the Next Step with Citi Footcare
If you are suffering from a fifth metatarsal base fracture and need expert surgical intervention, consider fifth metatarsal base fracture surgery at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved foot function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how fifth metatarsal base fracture surgery can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare
122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800
Beyond the Scalpel: Unleashing the Power of First Metatarsal Osteotomy in Bunion Correction
First Metatarsal Osteotomy
Bunions are a common yet often painful foot condition that affects many individuals. The discomfort and misalignment caused by bunions can significantly impact a person’s quality of life. Traditional bunion surgeries can be invasive and require extended recovery times. However, first metatarsal osteotomy has emerged as a powerful and effective method for bunion correction. This blog explores the benefits and effectiveness of first metatarsal osteotomy, highlighting why it might be the best option for those suffering from bunions.
Understanding Bunions and Their Impact
Bunions, medically known as hallux valgus, occur when the big toe deviates towards the other toes, creating a bony bump at the base of the toe. This deformity can cause pain, swelling, and difficulty in finding comfortable footwear. Factors contributing to bunion formation include genetic predisposition, wearing tight or ill-fitting shoes, and certain medical conditions such as arthritis.
The impact of bunions extends beyond physical discomfort. Many individuals with bunions experience reduced mobility and are forced to limit their activities. This can lead to a decreased quality of life, as everyday tasks and recreational activities become painful and challenging. For those with severe bunions, surgical intervention is often necessary to alleviate symptoms and restore foot function.
What is First Metatarsal Osteotomy?
First metatarsal osteotomy is a surgical procedure designed to correct the alignment of the first metatarsal bone, thereby addressing the underlying cause of bunions. The procedure involves making precise cuts in the first metatarsal bone to realign it properly. This realignment helps reduce the prominence of the bunion and corrects the toe’s deviation. The bone is then stabilized using screws or plates to ensure proper healing and alignment.
Benefits of First Metatarsal Osteotomy
The primary benefit of first metatarsal osteotomy is the significant improvement in foot alignment and reduction in pain. By addressing the root cause of the bunion deformity, this procedure provides lasting relief and enhances overall foot function. Patients who undergo first metatarsal osteotomy often experience a significant reduction in discomfort and are able to resume their daily activities without pain.
Another advantage of this procedure is the minimally invasive nature of the surgery. Modern surgical techniques allow for smaller incisions, resulting in less tissue damage and quicker recovery times. Patients typically experience less postoperative pain and can return to their normal activities sooner than with traditional bunion surgery.
Improved Quality of Life
For many patients, the decision to undergo first metatarsal osteotomy is driven by the desire to improve their quality of life. The ability to walk, run, and engage in physical activities without pain is a significant benefit of this procedure. Patients who have undergone first metatarsal osteotomy often report higher satisfaction levels due to the improved function and appearance of their feet.
The minimally invasive nature of the surgery also means that patients can enjoy a more comfortable recovery period. With less postoperative pain and swelling, individuals can return to work and their daily routines more quickly. This contributes to a better overall experience and a faster return to normal life.
Advances in Surgical Techniques
The success of first metatarsal osteotomy is largely due to advancements in surgical techniques and technology. Surgeons now have access to high-precision instruments and imaging tools that allow for better visualization and accuracy during the procedure. These innovations have made it possible to perform the surgery with a high degree of precision, leading to better outcomes and fewer complications.
The Expertise of Dr. Emanuel Sergi
At Citi Footcare, Dr. Emanuel Sergi and his team are at the forefront of performing first metatarsal osteotomy surgeries. With extensive training and experience in the latest surgical techniques, Dr. Sergi has helped countless patients achieve relief from bunion pain. His approach is personalized, taking into account each patient’s unique condition and lifestyle to develop a tailored treatment plan.
Dr. Sergi’s commitment to patient care extends beyond the operating room. He ensures that each patient receives comprehensive preoperative assessments and detailed postoperative care instructions. This holistic approach helps to maximize the success of the surgery and promotes optimal healing.
Who is a Candidate for First Metatarsal Osteotomy?
Not every patient with bunions will be a suitable candidate for first metatarsal osteotomy. The ideal candidates are typically those with moderate to severe bunion deformities that have not responded to conservative treatments such as orthotics, physical therapy, or medication. A thorough evaluation by a skilled podiatrist, like Dr. Emanuel Sergi at Citi Footcare, is essential to determine the most appropriate treatment plan.
Long-Term Success and Follow-Up Care
The long-term success of first metatarsal osteotomy depends on several factors, including the surgeon’s expertise, the patient’s adherence to postoperative care instructions, and any underlying health conditions. Regular follow-up visits are crucial to monitor healing and address any concerns promptly. Most patients can expect significant pain relief and improved foot function that lasts for years.
Patient Success Story: Emily’s Journey
Emily, an active professional in New York City, struggled with severe bunion pain that limited her daily activities and made finding comfortable shoes a nightmare. After consulting with Dr. Emanuel Sergi at Citi Footcare, Emily decided to undergo first metatarsal osteotomy. The surgery was a success, and within a few weeks, Emily noticed significant improvements. The pain had subsided, and she was able to walk and even jog without discomfort. Emily’s experience highlights the transformative potential of first metatarsal osteotomy and the exceptional care provided by Citi Footcare.
Why Citi Footcare is the Best Choice for First Metatarsal Osteotomy in New York City
Choosing the right podiatrist for first metatarsal osteotomy is crucial for achieving the best possible outcomes. Citi Footcare stands out as the premier choice for several reasons. The team at Citi Footcare, led by Dr. Emanuel Sergi, consists of highly experienced and skilled podiatrists who specialize in minimally invasive foot surgeries. They utilize the latest technology and surgical techniques to provide top-notch care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a proven track record of successful surgeries and satisfied patients who have experienced significant improvements in their quality of life. Located conveniently in the heart of New York City, Citi Footcare offers easy access to top-tier podiatric care.
Patient Success Story: Adya’s Path to Pain-Free Living
Adya, a dedicated teacher in New York City, had always been on her feet, guiding her students and engaging in activities with them. Over time, she began experiencing sharp pain in her big toe, which was later diagnosed as a severe bunion. The pain became unbearable, making it difficult for her to walk, stand, or even find suitable shoes. Desperate for a solution, Adya visited Citi Footcare and met with Dr. Emanuel Sergi.
During her initial consultation, Dr. Sergi conducted a thorough examination and recommended first metatarsal osteotomy as the best option to correct her bunion and alleviate the pain. Adya felt reassured by Dr. Sergi’s detailed explanation of the procedure and the expected outcomes. She decided to proceed with the surgery, confident in the expertise of the Citi Footcare team.
The surgery was a success. Dr. Sergi skillfully performed the first metatarsal osteotomy, realigning Adya’s toe and reducing the bunion. The recovery process was smooth, thanks to the minimally invasive nature of the procedure. Adya followed her postoperative care instructions diligently, and within a few weeks, she noticed a significant reduction in pain and swelling.
Adya’s positive experience at Citi Footcare transformed her life. She was able to return to her classroom, moving around with ease and participating in activities she had missed. The first metatarsal osteotomy not only relieved her pain but also restored her confidence and mobility. Adya’s journey highlights the exceptional care provided by Dr. Emanuel Sergi and the team at Citi Footcare, showcasing the life-changing impact of advanced bunion correction techniques.
Take the Next Step with Citi Footcare
If you are suffering from bunions and looking for a powerful and minimally invasive solution, consider first metatarsal osteotomy at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved foot function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how first metatarsal osteotomy can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare122 East 42nd Street Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
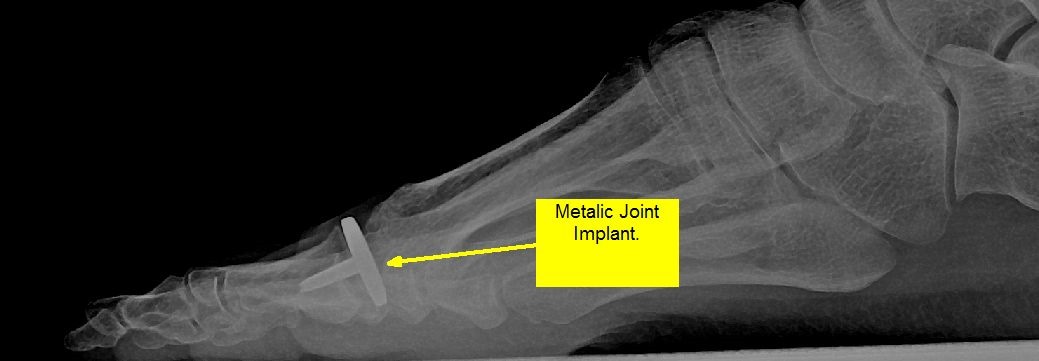
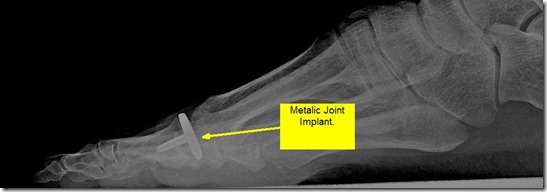
Beyond Fusion: Why First MPJ Implants Might Be Your Best Option
First MPJ Implants
When dealing with chronic pain and mobility issues in the big toe, patients often face a critical decision: fusion surgery or an implant. The first metatarsophalangeal (MPJ) joint is essential for everyday activities, and any surgical intervention must be carefully considered. First MPJ implants are emerging as a viable alternative to traditional fusion surgery, offering significant benefits that can enhance quality of life. This blog explores why first MPJ implants might be the best option for those suffering from severe arthritis or joint damage in the big toe.
Understanding First MPJ Implant Surgery
First MPJ implant surgery involves replacing the damaged joint with a prosthetic implant. This procedure aims to restore joint function and alleviate pain without permanently fusing the bones together. The implant mimics the natural joint, allowing for movement and flexibility. During the surgery, the damaged cartilage and bone are removed, and the implant is carefully positioned to ensure proper alignment and function.
Advantages of First MPJ Implants Over Fusion
One of the primary advantages of first MPJ implants is the preservation of joint movement. Unlike fusion, which permanently eliminates joint motion, implants allow patients to maintain a more natural gait and range of motion. This can be particularly beneficial for those who engage in activities that require foot flexibility, such as dancing or running.
Another significant advantage is the reduction in adjacent joint stress. Fusion can lead to increased pressure on the surrounding joints, potentially causing further complications down the line. Implants, by preserving joint movement, help distribute pressure more evenly across the foot, reducing the risk of additional problems.
Improved Quality of Life
For many patients, the prospect of maintaining joint movement is a major factor in choosing an implant over fusion. Being able to walk, run, and engage in physical activities without pain or stiffness can significantly improve overall quality of life. Patients who opt for implants often report higher satisfaction levels due to the natural feel and function of the prosthetic joint.
Advances in Implant Technology
Recent advancements in implant technology have made first MPJ implants more reliable and effective than ever before. Modern implants are designed to mimic the natural anatomy of the joint, providing a more comfortable and durable solution. Materials such as titanium and medical-grade polyethylene are commonly used, offering excellent biocompatibility and longevity.
Surgical Technique and Recovery
The surgical technique for first MPJ implants has also evolved, with minimally invasive approaches becoming more common. These techniques reduce recovery times and minimize post-operative complications. Patients typically experience less pain and swelling after surgery, allowing them to return to their normal activities sooner.
Recovery from first MPJ implant surgery involves a period of rest and rehabilitation. Physical therapy is often recommended to strengthen the foot and ensure proper healing. Most patients can expect to resume normal activities within a few months, with full recovery taking up to a year.
Long-Term Outcomes and Patient Satisfaction
Studies have shown that first MPJ implants can provide excellent long-term outcomes. Many patients report significant pain relief and improved function for years after the surgery. The success of the procedure largely depends on the surgeon’s expertise and the quality of the implant used. Regular follow-up visits are crucial to monitor the implant’s performance and address any issues promptly.
The Expertise of Dr. Emanuel Sergi
At Citi Footcare, Dr. Emanuel Sergi and his team of highly skilled podiatrists specialize in first MPJ implant surgery. With extensive experience and a commitment to patient care, they provide personalized treatment plans tailored to each patient’s unique needs. Dr. Sergi’s expertise ensures that patients receive the highest quality care and achieve the best possible outcomes.
Potential Risks and Considerations
As with any surgical procedure, first MPJ implant surgery carries certain risks. Potential complications include infection, implant loosening, and nerve damage. However, these risks are relatively low, especially when the surgery is performed by an experienced podiatrist. Patients should discuss all potential risks and benefits with their surgeon to make an informed decision.
Why Citi Footcare is the Best Choice for First MPJ Implants in New York City
Choosing the right podiatrist for first MPJ implant surgery is crucial for ensuring successful results. Citi Footcare stands out as the best choice for several reasons. The team at Citi Footcare includes some of the most experienced and highly trained podiatrists in New York City. They use state-of-the-art technology and advanced surgical techniques to provide the best possible care. Patients benefit from a comprehensive approach that includes pre-operative consultations, detailed surgical plans, and thorough post-operative care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a track record of successful surgeries and happy patients who have experienced significant improvements in their quality of life. With a convenient location in the heart of New York City, Citi Footcare makes it easy for patients to access top-tier podiatric care.
Take the Next Step with Citi Footcare
If you are suffering from pain or mobility issues related to the first metatarsophalangeal joint, consider first MPJ implant surgery at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how first MPJ implant surgery can benefit you and to discuss your treatment options with our expert team.
Patient Success Story: Sean’s Return to an Active Lifestyle
Sean, an avid runner and fitness enthusiast, found himself facing a debilitating issue. Persistent pain in his big toe had begun to hinder his daily runs and workouts. Over time, the pain grew so severe that even walking became a challenge. Desperate for a solution, Sean turned to Citi Footcare, seeking the expertise of Dr. Emanuel Sergi and his team.
During his initial consultation, Dr. Sergi conducted a thorough examination and determined that Sean had advanced arthritis in his first metatarsophalangeal (MPJ) joint. After discussing various treatment options, Dr. Sergi recommended first MPJ implant surgery as the best solution to restore Sean’s mobility and relieve his pain. The idea of maintaining joint movement while eliminating the pain appealed to Sean, and he decided to proceed with the surgery.
The procedure was a success. Dr. Sergi skillfully replaced the damaged joint with a state-of-the-art implant, ensuring proper alignment and function. Post-surgery, Sean followed a comprehensive rehabilitation plan that included physical therapy to strengthen his foot and regain full mobility. The support and guidance from the Citi Footcare team were instrumental in his recovery.
As weeks passed, Sean began to notice significant improvements. The pain that once plagued him was gone, and he gradually returned to his active lifestyle. He was able to run again, pain-free, and participate in fitness activities he had missed. The first MPJ implant not only relieved his pain but also allowed him to maintain the flexibility and movement necessary for his active routine.
Sean’s positive experience at Citi Footcare highlights the transformative potential of first MPJ implant surgery. His journey from debilitating pain to an active, pain-free life underscores the expertise and dedication of Dr. Emanuel Sergi and his team. Sean’s story is a testament to the life-changing impact of advanced podiatric care and the benefits of choosing Citi Footcare for first MPJ implant surgery.
If you are suffering from pain or mobility issues related to the first metatarsophalangeal joint, consider first MPJ implant surgery at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how first MPJ implant surgery can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare
122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800
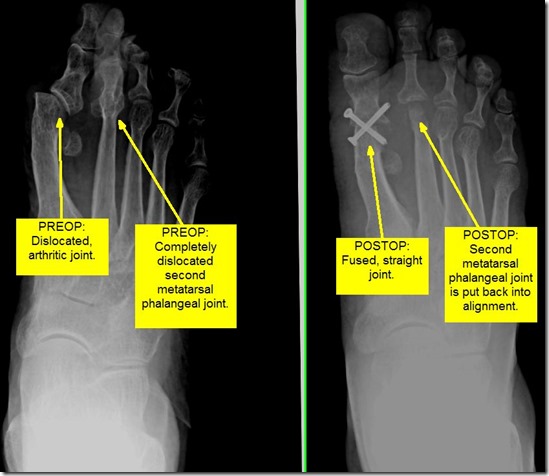
Step into the Future: Is First MTP Joint Fusion the Ultimate Solution?
Is First MTP Joint Fusion the Ultimate Solution?
The first metatarsal phalangeal (MTP) joint plays a crucial role in the movement and stability of the foot. It is essential for walking, running, and other activities. When this joint becomes damaged or arthritic, it can lead to significant pain and mobility issues. First MTP joint fusion surgery has emerged as a potential solution, offering relief to many patients. This blog explores whether this procedure is the ultimate solution for MTP joint problems.
Understanding First MTP Joint Fusion Surgery
First MTP joint fusion surgery involves the fusion of the bones in the big toe joint. The goal is to eliminate the arthritic joint, thus reducing pain and improving function. During the procedure, the surgeon removes the damaged cartilage and aligns the bones in a corrected position. These bones are then fixed together using plates, screws, or other hardware until they heal into one solid bone.
Benefits of First MTP Joint Fusion Surgery
One of the primary benefits of first MTP joint fusion surgery is pain relief. Patients suffering from severe arthritis or deformities in the big toe joint often experience significant pain relief post-surgery. The fusion of the joint eliminates the movement that causes pain, allowing patients to return to their daily activities without discomfort.
Improved Function and Mobility
Another significant advantage of this surgery is improved function and mobility. By stabilizing the joint, the fusion allows patients to walk more comfortably and engage in physical activities that were previously difficult or impossible. The surgery can correct deformities, improve the alignment of the foot, and enhance overall stability.
Longevity of the Results
First MTP joint fusion surgery offers long-lasting results. Unlike other treatments that may require repeated interventions, the fusion provides a permanent solution. Once the bones heal, they remain fused, and patients can enjoy the benefits for many years without the need for additional procedures.
Potential Drawbacks and Considerations
While first MTP joint fusion surgery has many benefits, it is important to consider potential drawbacks. The fusion eliminates the movement of the joint, which can affect certain activities such as running or dancing. Patients may need to adjust their footwear and activities post-surgery. Additionally, there is a recovery period during which patients must avoid putting weight on the foot to allow proper healing.
Alternatives to First MTP Joint Fusion Surgery
For some patients, alternatives to first MTP joint fusion surgery may be more appropriate. These alternatives include joint replacement, where the damaged joint is replaced with an artificial implant, or conservative treatments such as orthotics, physical therapy, and medication. Each treatment option has its own set of advantages and potential drawbacks, and the best choice depends on the individual patient’s condition and lifestyle.
Advances in Surgical Techniques
Advancements in surgical techniques and technology have made first MTP joint fusion surgery more effective and less invasive. Minimally invasive procedures, improved fixation devices, and enhanced imaging techniques have all contributed to better outcomes for patients. These advancements have reduced recovery times, minimized complications, and improved overall patient satisfaction.
Patient Success Stories
Hearing from patients who have undergone first MTP joint fusion surgery can provide valuable insights and encouragement. Many patients report significant improvements in their quality of life following the procedure. For instance, individuals who struggled with chronic pain and limited mobility often find that they can return to activities they once enjoyed, such as walking, hiking, or even playing sports. These success stories highlight the transformative potential of the surgery.
Post-Surgery Care and Rehabilitation
Post-surgery care is critical to ensure the success of first MTP joint fusion surgery. Patients must follow their surgeon’s instructions closely, which typically includes a period of non-weight bearing to allow the bones to heal properly. Physical therapy may also be recommended to strengthen the surrounding muscles and improve overall foot function. Proper care and rehabilitation can significantly enhance the long-term outcomes of the surgery.
The Role of Customized Orthotics
Customized orthotics can play a supportive role in the recovery and long-term management of patients who undergo first MTP joint fusion surgery. These devices are designed to provide additional support and alignment to the foot, helping to distribute pressure evenly and reduce strain on the fused joint. Orthotics can be particularly beneficial for patients who engage in high-impact activities or have other foot-related conditions.
The Expertise of Dr. Emanuel Sergi
At Citi Footcare, Dr. Emanuel Sergi and his team of highly skilled podiatrists specialize in first MTP joint fusion surgery. With extensive experience and a commitment to patient care, they provide personalized treatment plans tailored to each patient’s unique needs. Dr. Sergi’s expertise ensures that patients receive the highest quality care and achieve the best possible outcomes.
Why Citi Footcare is the Best Choice for First MTP Joint Fusion Surgery in New York City
Choosing the right podiatrist for first MTP joint fusion surgery is crucial for ensuring successful results. Citi Footcare stands out as the best choice for several reasons. The team at Citi Footcare includes some of the most experienced and highly trained podiatrists in New York City. They use state-of-the-art technology and advanced surgical techniques to provide the best possible care. Patients benefit from a comprehensive approach that includes pre-operative consultations, detailed surgical plans, and thorough post-operative care.
Citi Footcare’s commitment to patient satisfaction and positive outcomes is unmatched. The practice has a track record of successful surgeries and happy patients who have experienced significant improvements in their quality of life. With a convenient location in the heart of New York City, Citi Footcare makes it easy for patients to access top-tier podiatric care.
Patient Success Story: Miranda’s Journey to Pain-Free Living
Miranda, a vibrant and active New Yorker, had always enjoyed exploring the city’s parks and taking long walks along the Hudson River. However, over time, she began experiencing excruciating pain in her big toe. The pain became so intense that it started to affect her daily life, making even short walks unbearable. Frustrated and desperate for relief, Miranda decided to seek help at Citi Footcare.
During her initial consultation, Miranda met with Dr. Emanuel Sergi, who carefully listened to her concerns and thoroughly examined her condition. After a detailed discussion about her symptoms and lifestyle, Dr. Sergi diagnosed her with severe arthritis in the first metatarsal phalangeal (MTP) joint. He explained that first MTP joint fusion surgery could be the ideal solution to alleviate her pain and restore her mobility.
Feeling hopeful, Miranda agreed to proceed with the surgery. The team at Citi Footcare guided her through every step of the process, ensuring she felt comfortable and informed. On the day of the surgery, Miranda was greeted with warm smiles and reassurance from the staff. The procedure went smoothly, and Dr. Sergi skillfully performed the fusion, aligning the bones perfectly.
The post-surgery period required patience and dedication. Miranda followed Dr. Sergi’s instructions meticulously, attending physical therapy sessions and gradually increasing her activity levels. The team at Citi Footcare provided unwavering support, answering her questions and offering encouragement throughout her recovery.
As the weeks passed, Miranda noticed a remarkable improvement. The pain that once plagued her was gone, replaced by a newfound sense of freedom. She could walk longer distances without discomfort and even resumed her beloved strolls along the Hudson River. The successful first MTP joint fusion surgery had transformed her life, allowing her to embrace an active lifestyle once again.
Miranda’s journey is a testament to the expertise and compassionate care provided by Dr. Emanuel Sergi and the team at Citi Footcare. Her positive experience highlights the life-changing potential of first MTP joint fusion surgery and underscores why Citi Footcare is the best choice for patients seeking relief from foot pain in New York City.
Take the Next Step with Citi Footcare
If you are suffering from pain or mobility issues related to the first metatarsal phalangeal joint, consider first MTP joint fusion surgery at Citi Footcare. Dr. Emanuel Sergi and his team are dedicated to helping patients achieve pain relief and improved function through advanced surgical techniques and personalized care. Schedule a consultation today to learn more about how first MTP joint fusion surgery can benefit you and to discuss your treatment options with our expert team.
Contact us at:
Citi Footcare122 East 42nd Street Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
The Definitive Choice for Hammertoe Fusion Success: Screw It!
Unlocking Hammertoe Fusion Success with Screw Fixation
In the bustling metropolis of New York City, where every step counts, foot health is paramount. Hammertoes, a common foot deformity characterized by abnormal bending of the toe joints, can significantly impact one’s quality of life. For individuals seeking relief from hammertoe discomfort, hammertoe fusion surgery emerges as a viable solution. In podiatric surgical treatment, the choice of fixation method plays a crucial role in determining the success of the procedure. Among the various options available, screw fixation stands out as the definitive choice for hammertoe fusion success.
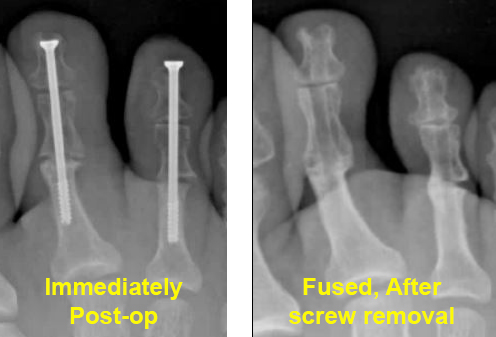 Before and after hammertoe surgery. arthrodesis.
Before and after hammertoe surgery. arthrodesis.
What is a Hammertoe?
A hammertoe is a deformity that occurs when one of the toe joints bends abnormally, causing the toe to resemble a hammer. This condition can be painful and make walking difficult. Hammertoes can result from wearing ill-fitting shoes, foot injuries, or underlying foot problems such as arthritis or muscle imbalance.
Understanding Hammertoe Fusion Surgery
Hammertoe fusion surgery, also known as arthrodesis, aims to correct the deformity by fusing the affected toe joints in a straightened position. This procedure not only alleviates pain and discomfort but also restores proper alignment, allowing patients to regain mobility and function in their toes. Successful hammertoe fusion relies heavily on achieving stable fixation of the toe joints, which is where the choice of fixation method becomes pivotal.
The Superiority of Screw Fixation
Screw fixation involves the use of specialized screws to stabilize the toe joints during hammertoe fusion surgery. Unlike traditional methods such as K-wires, screws offer enhanced stability and durability, resulting in better long-term outcomes for patients. Research published in scientific journals, such as the article titled “Hammertoe Arthrodesis with Screw Versus Kirschner Wire Fixation: A Systematic Review and Meta-analysis” by Malik et al., highlights the advantages of screw fixation over alternative methods.
Advantages of Screw Fixation in Hammertoe Fusion
- Enhanced Stability: Screws provide a secure anchor for the toe joints, promoting proper alignment and reducing the risk of recurrence.
- Improved Fusion Rate: The design of screws facilitates better bone-to-bone contact, leading to faster and more reliable fusion.
- Reduced Risk of Complications: Screw fixation minimizes the risk of complications such as migration or breakage, ensuring a smoother recovery process.
- Long-Term Durability: Screws are designed to remain in place permanently, offering lasting relief from hammertoe deformity without the need for further intervention.
- Faster Recovery: With screws, patients typically experience a faster recovery compared to other fixation methods, enabling them to return to their normal activities sooner.
Opting for Citi Footcare: The Top Choice for Hammertoe Fusion Surgery in NYC
At Citi Footcare, we understand the importance of effective hammertoe fusion surgery in improving our patients’ quality of life. Led by Dr. Emanuel Sergi and a team of experienced podiatrists, we specialize in performing hammertoe fusion surgery using screw fixation techniques. Our state-of-the-art facility, Gramercy Surgery Center, combined with our expertise and personalized approach to patient care, sets us apart as the premier choice for podiatric treatment in New York City.
Comprehensive Care for Lasting Relief
When you choose Citi Footcare for your hammertoe fusion surgery, you can expect comprehensive care from start to finish. Our team will conduct a thorough evaluation to assess your condition and determine the most appropriate treatment plan. Throughout the surgical process, we prioritize patient comfort and safety, ensuring that you feel supported every step of the way. After surgery, we provide attentive post-operative care to monitor your progress and address any concerns that may arise.
The Importance of Patient Education
At Citi Footcare, we believe in the power of patient education. We take the time to thoroughly explain the hammertoe fusion procedure, including the benefits of screw fixation, to ensure that our patients feel informed and empowered to make confident decisions about their care. By fostering open communication and providing clear, understandable information, we aim to create a partnership with our patients based on trust and mutual respect.
Continued Support and Follow-Up Care
Our commitment to our patients extends beyond the operating room. We provide ongoing support and follow-up care to ensure that you achieve the best possible outcome from your hammertoe fusion surgery. Whether you have questions or concerns during your recovery period or require additional treatment in the future, our team is here to provide the expert care and guidance you need to maintain healthy, pain-free feet.
Take the First Step Towards Lasting Relief
If you’re experiencing discomfort from hammertoe deformity and seeking a definitive solution for lasting relief, schedule a consultation with Dr. Emanuel Sergi and the expert podiatrists at Citi Footcare. Reclaim your mobility and quality of life today.
Citi Footcare
122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
Going Toe-to-Toe: Fusion vs. Arthroplasty for Hammertoe + Case study of digital Arthrodesis (Fusion) with Before and after pictures
Going Toe-to-Toe: Fusion vs. Arthroplasty for Hammertoe
Navigating the complex landscape of hammertoe treatment, patients are often presented with a pivotal choice between two leading surgical interventions: fusion, also known as arthrodesis, and arthroplasty. Each modality offers distinct advantages and considerations, making the decision process highly individualized. This detailed exploration aims to shed light on both treatments, equipping you with the knowledge to make an informed choice.
What is a Hammertoe?
Hammertoe is a common foot deformity that affects the alignment of one or more toes, causing them to bend at the middle joint and resemble a hammer or a claw. This condition often arises from an imbalance in the muscles, tendons, and ligaments that normally hold the toe straight. Over time, the persistent bending can lead to stiffness and pain, particularly when wearing shoes, as the toe’s raised position leads to friction and pressure. Factors contributing to the development of hammertoe include genetics, arthritis, wearing ill-fitting shoes, and trauma. Recognizing the early signs of hammertoe is crucial for effective management and treatment, as the condition can become progressively worse, leading to significant discomfort and limitations in foot function.
Demystifying Hammertoe
Hammertoe manifests as a noticeable bend at the middle joint of the toe, causing it to adopt a downward curl rather than extending straight out. This condition frequently stems from an imbalance in the muscular and tendon structures of the foot, leading to sustained pressure on the toe’s tendons and joints. As the condition progresses, the toe’s abnormal posture becomes more pronounced, often resulting in significant discomfort, pain, and challenges in mobility.
The Fusion Solution: Arthrodesis Explained
Arthrodesis stands out as a definitive solution for advanced hammertoe cases, entailing the surgical fusion of the joint to rectify the deformity. The procedure involves excising a segment of the affected joint and securing the adjacent bones into a corrected position using hardware such as pins or screws. While this method guarantees a permanent fix and significant stability, it does compromise the joint’s natural flexibility, which may not align with the preferences or requirements of all patients.
Arthroplasty: Preserving Flexibility
Contrastingly, arthroplasty offers an alternative approach by excising the deformed part of the joint and, if necessary, incorporating an implant or modifying the remaining bone structure to realign and restore the toe’s functionality. This technique is particularly valued for its ability to maintain a degree of the toe’s inherent mobility, catering to patients who prioritize functional flexibility alongside corrective outcomes.
Evaluating Outcomes: Fusion vs. Arthroplasty
The choice between arthrodesis and arthroplasty hinges on a careful assessment of the patient’s specific condition, lifestyle, and treatment objectives. Arthrodesis delivers a lasting solution with minimal risk of recurrence but at the cost of joint movement. Arthroplasty, while preserving movement, may not offer the same level of stability as fusion, making it a more suitable option for individuals who value flexibility.
The Role of Patient Education and Tailored Treatment
An essential aspect of hammertoe management is patient education, empowering individuals to make informed decisions regarding their treatment. Understanding the nuances of each surgical option, including the potential risks, recovery times, and long-term outcomes, is crucial. A personalized treatment plan, developed in collaboration with a skilled podiatrist, can significantly enhance the effectiveness of the chosen intervention and the overall patient experience.
Why Citi Footcare is the Best Choice for Hammertoe Treatment in New York City
At Citi Footcare, under the distinguished leadership of Dr. Emanuel Sergi, we pride ourselves on being at the vanguard of hammertoe treatment in the metropolitan landscape. Our clinic is celebrated for its individualized patient care approach, ensuring that treatment regimens are precisely tailored to align with each patient’s unique needs and aspirations.
Our clinic is outfitted with cutting-edge podiatric technology, empowering us to provide the most advanced surgical options for hammertoe, encompassing both fusion and arthroplasty. Dr. Sergi’s unparalleled expertise, combined with our team’s in-depth understanding of foot biomechanics, positions us to achieve superior treatment outcomes, facilitating a swift and comfortable return to everyday activities for our patients.
Hammertoe Case study of digital Arthrodesis (Fusion) with Before and after pictures
Below are before and after pictures of a patient with severely painful, contracted hammertoes, bilaterally. We chose to perform a digital arthrodesis, fusion, of toes 2 and 3 in order to permanently fix the hammertoes such that they will not come back in the future. This patient underwent fusion of the second and third toes with tendon lengthening in order to bring the toes down.
Pre-op photos
Post-op photos
Final Thoughts and Next Steps
If you are grappling with the challenges of hammertoe, let Citi Footcare be your partner in navigating the path to recovery. Dr. Emanuel Sergi, along with our accomplished team of podiatrists, is dedicated to supporting you through every phase of the decision-making and treatment process.
We invite you to reach out and schedule a consultation to explore how we can tailor a treatment plan to your specific needs, ensuring a journey to recovery that is both effective and aligned with your lifestyle. Discover why Citi Footcare is the pinnacle of podiatric care in New York City.
Citi Footcare122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800
A Journey to Comfort: Camille’s Transformation with Scarf Osteotomy with before and after pictures
Understanding Bunions: The First Step to Relief
Bunions, or Hallux Valgus, emerge as bony protrusions at the base of the big toe, resulting from the misalignment of the toe’s joints. This condition not only brings about discomfort and pain but also significantly affects mobility and quality of life. Factors contributing to bunions range from genetic predispositions to unsuitable footwear choices, leading to a pressing need for effective treatment options.
Before and after pictures Scarf Bunionectomy


The Crucial Decision: Opting for Bunion Surgery
Surgery becomes a pivotal choice when non-invasive treatments fail to alleviate the discomfort caused by bunions. The goal of surgical intervention is to rectify the deformity, mitigate pain, and enhance foot functionality, ultimately restoring the patient’s quality of life. This step is especially vital for individuals enduring severe pain, mobility challenges, and a noticeable decline in life quality.
Camille’s Story: A New York Tale of Recovery and Renewal
Camille (name changed for privacy), a dynamic individual from New York City, found her vibrant lifestyle hindered by a debilitating bunion. Her quest for relief led her to Citi Footcare, where Dr. Emanuel Sergi recommended the innovative Scarf Osteotomy procedure. This marked the beginning of Camille’s transformative journey.
Complementary Precision: The Role of Akin Osteotomy
Scarf Bunionectomy stands as a permanent solution for those grappling with severe bunion deformities. This surgical technique involves a strategic Z-shaped incision in the metatarsal bone, enabling precise realignment. Its unparalleled stability and corrective capability make it a preferred choice for comprehensive bunion correction.
The Innovative Approach: Scarf Bunionectomy
Often paired with Scarf Osteotomy, the Akin Osteotomy procedure fine-tunes the alignment by adjusting the phalanx of the big toe. This additional step is instrumental for patients with pronounced angular disparities between their toes, ensuring a thorough and holistic correction.
Camille’s Surgical Journey: A Dual Approach to Restoration
For Camille, the combined procedures of Scarf and Akin Osteotomy offered the most promising path to recovery. The two-screw fixation technique in the Scarf Osteotomy ensured unmatched stability, while the Akin Osteotomy meticulously aligned her toe, addressing her bunion deformity comprehensively. Due to cysts discovered during surgery, decision was made to add 2 crossed K wires for additional fixation.
Navigating Recovery: A Structured Path to Healing
Post-operative care is pivotal for achieving the desired surgical outcomes. Camille adhered to a stringent recovery protocol, starting with three days of non-weight bearing, followed by a four-week period in a cam walker. This regimented approach facilitated optimal healing, minimized discomfort, and curbed swelling, paving the way for a successful recovery.
Why Scarf Osteotomy Outshines Austin Bunionectomy
The debate between Scarf Osteotomy and Austin Bunionectomy often centers on their effectiveness and long-term outcomes. The Scarf procedure, with its intricate Z-shaped osteotomy, allows for comprehensive proximal angular correction, offering a more tailored correction compared to the singular bone cut of the Austin method. This not only ensures enhanced stability but also significantly reduces the chances of recurrence, positioning the Scarf Osteotomy as the superior choice for enduring relief.
Camille’s Experience: A Testament to Transformation
Camille’s journey from discomfort to renewal is a testament to the efficacy of the Scarf Osteotomy combined with Akin Osteotomy. Her experience highlights the importance of personalized care and advanced surgical techniques in addressing complex bunion deformities. From the initial consultation to the meticulous post-operative care, Camille’s story is one of hope, resilience, and the promise of a pain-free future.
Why Citi Footcare is Your Ally in Bunion Treatment
At Citi Footcare, under the guidance of Dr. Emanuel Sergi and our team of experienced podiatrists, we pride ourselves on delivering state-of-the-art bunion treatment. Our commitment to utilizing advanced procedures like the Scarf Osteotomy ensures our patients receive the most effective and personalized care. Our success stories, like Camille’s, underscore our position as the leading podiatry practice in New York City for those seeking relief from bunion discomfort.
Embark on Your Journey to Comfort with Citi Footcare
If you, like Camille, are seeking an end to the pain and limitations caused by bunions, let Citi Footcare be your guide. With Dr. Emanuel Sergi and our dedicated team, you can embark on a journey towards a comfortable and active life. Reach out to us today to explore your treatment options and take the first step towards walking in comfort once again.
Citi Footcare
122 East 42nd Street Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
A Patient That Came in for Bunion Surgery: The Scarf Osteotomy Approach, including before and after pictures of bunion surgery.
Sheila’s Story: Seeking Relief from Bunion Pain
In the bustling heart of New York City, Sheila faced a challenge that affects millions: a painful bunion. This condition, more than just a cosmetic issue, impacted her daily life and comfort. Determined to find a lasting solution, Sheila turned to the renowned podiatry experts at Citi Footcare, a practice celebrated for its innovative approach to foot care.
Understanding Bunions: More Than Just a Foot Deformity
Bunions, medically known as hallux valgus, occur when the first metatarsal bone of the foot turns outward (first metatarsal varus) while the big toe points inward towards the other toes. This misalignment results in a prominent bony bump on the side of the foot and can lead to significant pain and discomfort. Over time, the condition can worsen, leading to chronic pain and mobility issues.
Preoperative Photo:
Here you can clearly see the bunion deformity where the first metatarsal bone has moved medially to stick out on the inside of the patient’s foot.

First Metatarsal Varus and Hallux Valgus: A Closer Look
The condition starts with the first metatarsal bone moving in a varus position, causing the toe to angle in a valgus position. This movement not only affects the joint at the base of the big toe but can also lead to secondary issues such as corns, calluses, and hammertoes. Understanding this underlying pathology is crucial in determining the most effective treatment approach.
Choosing the Scarf Osteotomy for Bunion Correction
After careful evaluation at Citi Footcare, the decision was made to proceed with a scarf osteotomy for Sheila. This decision was based on the nature of her bunion deformity and her overall foot structure. At Citi Footcare, we often use the scarf osteotomy, despite being technically more difficult and other osteotomies, in order to address the deformity more proximal at its origin. The scarf osteotomy is far superior to more distal osteotomies that are commonly performed by most foot surgeons.
The Scarf Osteotomy Procedure: A Detailed Walkthrough
The scarf osteotomy is our preferred surgical method for bunion correction due to its effectiveness and stability. This procedure involves a series of intricate steps:
- Incision and Exposure: A precise incision is made along the side of the foot to expose the metatarsal bone.
- Bone Cutting: The metatarsal bone is cut in a Z-shape (scarf cut), allowing for multiplanar correction of the deformity.
- Bone Realignment: The segments of the bone are shifted to realign the toe and correct the varus position of the metatarsal.
- Fixation: Two screws are strategically placed to secure the bone in its new position, ensuring stability and promoting proper healing.
- Closure: The incision is meticulously closed with a plastic surgery type method, and a dressing is applied to protect the surgical site.
Postoperative Photo 1:
Here you can clearly see the bunion deformity is gone. This photo was taken to months after surgery. You can see there is still swelling noted to the entire forefoot. Note that there is a relatively straight line the tip of first toe back to the midfoot. This is in contrast to the preoperative photo where a large bump is present.

Postoperative Photo 2:
On this side view photo, note the well-healed incision despite being only 8 weeks after surgery. This is achieved warming a plastic surgery type suture technique. You can also see at the distal end of the incision there is a vertical component that is about 90° to the main part of the incision. Here, a skin plasty was performed to remove a triangle-shaped area of skin in order to remove excess skin that was present due to the bunion deformity.

Post-Surgical Recovery: Journey Toward Mobility
Sheila’s recovery was carefully monitored by the experts at Citi Footcare. The post-surgical phase is critical and involves several stages:
- Immediate Post-Op: Initial days focus on rest, ice, compression, and elevation to reduce swelling and pain. Patients are requested to stay off their feet the first 3 days. They will wear a surgical boot for around 4 weeks.
- Rehabilitation: Gradual off-weight-bearing exercises, followed by weight during exercise are introduced to aid in recovery.
- Follow-Up Care: Regular check-ups ensure proper healing and alignment of the toe. We continue to see our patient periodically for up to one year surgery.
Expected Recovery Times and Activity Restrictions
Typically, patients can expect to return to normal activities within 6 to 8 weeks post-surgery. However, full recovery, including the resumption of high-impact activities, may take up to 3-6 months. During this period, patients are advised to wear comfortable footwear and avoid strenuous activities to facilitate healing.
Long-Term Success: Relief from Bunion Pain
The long-term outcomes of a scarf osteotomy are highly favorable. Patients like Sheila experience significant relief from bunion pain and improved foot function. This procedure not only corrects the physical deformity but also enhances the quality of life by allowing a return to normal activities without discomfort.
Why Citi Footcare is the Best Choice in New York City
Citi Footcare, led by Dr. Emanuel Sergi and a team of skilled podiatrists and podiatric surgeons, is renowned for its expertise in treating foot conditions like bunions. The clinic’s state-of-the-art facilities, coupled with a patient-centric approach, make it the preferred choice for individuals seeking high-quality podiatric care. With a track record of successful outcomes and personalized treatment plans, Citi Footcare stands out as the leading podiatry practice in New York City.
Seeking Podiatry Treatment and Bunoin Surgery at Citi Footcare
For those suffering from foot conditions like bunions, Citi Footcare offers comprehensive treatment solutions. Under the guidance of Dr. Emanuel Sergi and his team, patients receive the highest standard of care. Reach out to Citi Footcare today to embark on a journey toward pain-free feet and improved mobility.
Citi Footcare122 East 42nd Street
Suite 2901
(E 42nd and Lexington Ave)
New York, NY 10168
212-871-0800
Tailor’s Bunion Surgery: A Transformative Journey at Citi Footcare
The Story of Jackie and Her Tailor’s Bunion.
Preoperative and postoperative photos below.
In the bustling city of New York, where every step on the vibrant streets counts, a patient named Jackie found herself struggling with an all-too-common yet often overlooked foot ailment. Jackie, an active New Yorker with a zest for life, faced a painful obstacle – a tailor’s bunion that impeded her daily activities and love for evening jogs in Central Park.
As Jackie researched her condition, she realized the importance of seeking professional help and chose Citi Footcare, a leading podiatry practice known for its successful outcomes and patient-centered approach. Her journey to recovery began the moment she stepped through the doors of this esteemed clinic.

Understanding Tailor’s Bunions
Before delving into the specifics of Jackie’s surgery, it is essential to understand what a tailor’s bunion is. This bony prominence, also known as a bunionette, forms on the outside base of the little toe. It occurs when the fifth metatarsal bone diverges from its normal alignment, creating pressure points and leading to pain and discomfort, especially when wearing shoes.
Patients like Jackie often find that tailor’s bunions can significantly impact their quality of life, leading them to seek surgical options after conservative treatments have been exhausted.
The Decision to Undergo Surgery
Jackie’s decision to undergo surgery was not made lightly. She had tried various non-invasive treatments, from padding to orthotics, but the pain persisted. After consultation with Dr. Emanuel Sergi and the expert team at Citi Footcare, Jackie felt confident in her choice. The team’s compassionate communication, coupled with their expertise in podiatry, assured her that she was in good hands.
 Jackie’s Pre-op Tailors Bunion
Jackie’s Pre-op Tailors BunionFifth Metatarsal Wedge Osteotomy with Screw Fixation: A Detailed Look
Jackie’s tailor’s bunion surgery involved a precise and advanced procedure known as the fifth metatarsal wedge osteotomy with screw fixation. This surgical technique is designed to correct the alignment of the fifth metatarsal bone.
The procedure entailed making an incision benind the fifth toe. Dr. Sergi then performed an osteotomy, which involves cutting and removing a wedge-shaped piece of bone from the fifth metatarsal. This realignment allowed for the correction of the bunionette deformity.
To secure the newly aligned bone, screw fixation was employed. This involved the insertion of a small titanium screw to hold the bone in its correct position. The use of screw fixation ensures stability during the healing process and helps maintain the correction over time.
Post-Surgical Care and Recovery
Jackie’s surgery was only part of her journey to recovery. Post-operative care is crucial for a successful outcome. Citi Footcare provided Jackie with an individualized recovery plan, including instructions for rest, ice, compression, and elevation (RICE), as well as a schedule for follow-up visits. She wore a surgical boot for 4 weeks after the surgery to protect the bone while it healed.
The dedicated staff also educated Jackie on how to manage post-surgical care at home, ensuring her path to recovery was clear and manageable. This entailed keeping her foot dry for a week after the surgery using a shower bag. She was given pain medication although she did not need much of it. Dr. Sergi uses multiple unique techniques to reduce postoperative pain. Their attentive follow-up and support played a significant role in Jackie’s healing process.
 Jackie’s Post-op Tailors Bunion
Jackie’s Post-op Tailors BunionThe Road to Recovery: Jackie’s Experience
Recovery from a fifth metatarsal wedge osteotomy with screw fixation typically involves a period of non-weight-bearing for a few days, followed by a transition to walking with a boot for support. Jackie adhered to the recovery plan, finding solace in the fact that each day brought her one step closer to a pain-free life.
She appreciated the comprehensive aftercare provided by Citi Footcare, where every follow-up visit showed progress and every question she had was met with an informative and reassuring response.
The Impact of Tailor’s Bunion Surgery on Quality of Life
As the weeks passed, Jackie noticed a profound improvement in her condition. The surgical correction of her tailor’s bunion allowed her to wear her favorite shoes again without discomfort. More importantly, she was able to return to her active lifestyle, participating in the New York City Marathon, a dream she thought was lost to her condition.
The surgery not only alleviated her physical pain but also restored her emotional well-being. Jackie’s journey with Citi Footcare was a testament to how a specialized surgical approach can profoundly impact a patient’s quality of life.
Why Citi Footcare is the Best Choice for Tailor’s Bunion Surgery in New York City
When it comes to addressing complex foot conditions like tailor’s bunions, New Yorkers seek the best possible care. Citi Footcare stands out as the premier podiatry practice for such procedures. With a team led by Dr. Emanuel Sergi, the clinic offers a blend of expert surgical skills, cutting-edge techniques, and a personalized approach to patient care.
Patients benefit from the practice’s use of the latest technology in diagnosis and treatment, including the fifth metatarsal wedge osteotomy with screw fixation procedure. This method, executed with precision and care, results in optimal outcomes and minimal downtime.
Moreover, Citi Footcare’s reputation for exceptional patient support throughout the treatment journey makes them the unequivocal choice for those seeking relief from tailor’s bunions and other foot-related concerns. Their commitment to patient education and comprehensive post-operative care ensures that individuals like Jackie not only recover but thrive following their surgical experience.
Experience the Citi Footcare Difference
Are you struggling with a tailor’s bunion or any other foot ailment? Do not let foot pain hold you back from the life you love. At Citi Footcare, Dr. Emanuel Sergi and the team of expert podiatrists are ready to help you take the next step towards pain-free living. With a successful track record in tailor’s bunion surgery and a patient-first philosophy, you can trust that your feet are in the best hands in New York City.
Contact us to schedule your appointment and start your journey to recovery. Our team is dedicated to providing you with the highest standard of podiatric care, tailored to your unique needs.
Citi Footcare122 East 42nd Street
Suite 2901
(E 42nd and Lexigton Ave)
New York, NY 10168
212-871-0800 https://www.CitiFootcare.com
citifootcare@gmail.com
Suffering from Heel Pain? NYC’s Ultimate Solution Will Amaze You!
Treatment for Plantar Fasciitis in NYC
In the bustling metropolis of New York City, where every step holds the promise of a new adventure, there’s one thing you shouldn’t have to worry about: heel pain. The constant throbbing and discomfort can put a damper on even the most exciting of plans. But fear not, because relief is closer than you think. Prepare to be astonished by the remarkable solution that awaits you at Citi Footcare, a leading podiatry practice that’s transforming lives one pain-free step at a time.
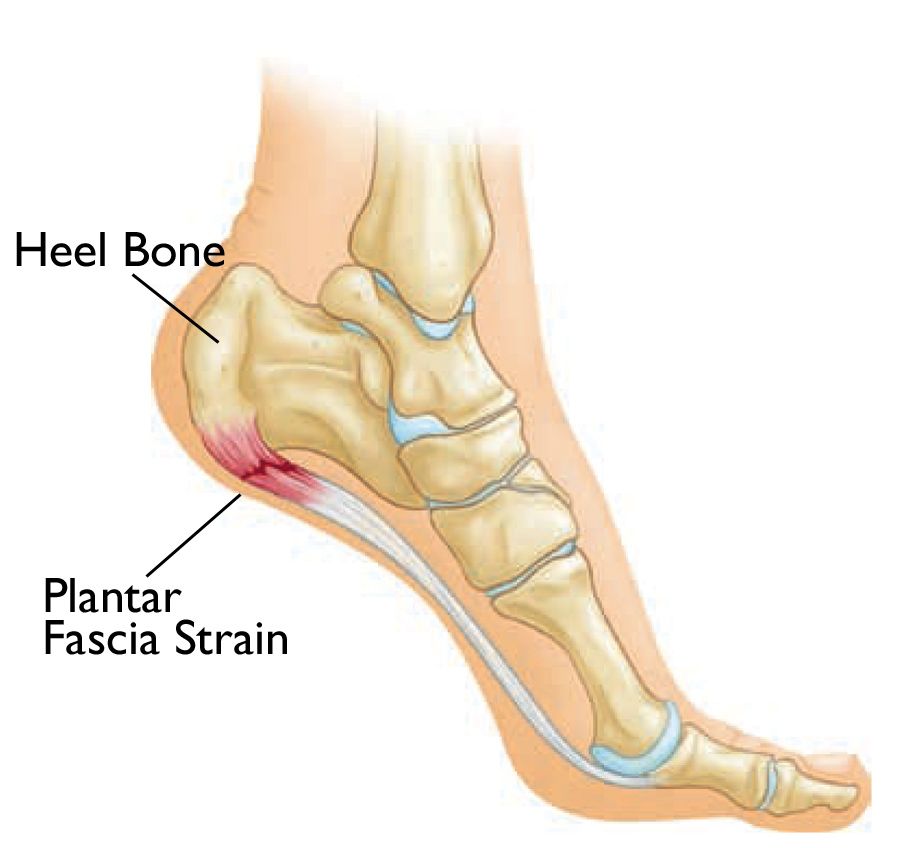
Understanding the Agony: Decoding the Causes of Heel Pain
Heel pain, as many unfortunate souls have experienced, can range from a dull ache to a sharp, shooting agony that makes you want to stop dead in your tracks. Two common culprits that lead to this torment are plantar fasciitis and Achilles tendonitis. Plantar fasciitis is all about inflammation – that tissue connecting your heel bone to your toes becomes inflamed, and every step feels like a struggle. Achilles tendonitis, on the other hand, involves the inflammation of the Achilles tendon at the back of your heel, causing yet another level of misery. It’s a double whammy that can turn your daily routine into a nightmare.
Enter Citi Footcare: Elevating Podiatry in the Concrete Jungle
Amid the towering skyscrapers and bustling streets of NYC, Citi Footcare emerges as a beacon of hope for those seeking refuge from heel pain. At the helm of this extraordinary practice is the esteemed podiatrist, Dr. Emanuel Sergi, a name synonymous with excellence and compassion. Dr. Sergi’s unwavering commitment to providing top-tier podiatric care has garnered Citi Footcare a reputation that echoes through the city’s avenues.
A Multifaceted Approach: The Science Behind Citi Footcare’s Success
Citi Footcare’s success in tackling heel pain is no magic trick – it’s the result of cutting-edge science combined with the art of personalized care. What sets them apart is their understanding that each foot is unique and, therefore, requires a tailored approach. Their arsenal of advanced techniques includes state-of-the-art orthotic devices designed to provide your feet with the support they crave. But that’s not all – shockwave therapy takes center stage, a revolutionary treatment that stimulates your body’s healing mechanisms, coaxing your pain away.
What is Plantar Fasciitis? Understanding the Culprit
Plantar fasciitis, a common cause of heel pain, is a condition characterized by the inflammation of the plantar fascia – the thick band of tissue that connects your heel bone to your toes. This inflammation can lead to stabbing pain in the bottom of your foot, especially when you take your first steps in the morning. Plantar fasciitis often occurs due to overuse, flat feet, high arches, or wearing improper footwear.
What Causes Plantar Fasciitis? Unraveling the Triggers
Plantar fasciitis can be triggered by various factors, including excessive physical activity, sudden weight gain, spending prolonged periods on your feet, and even wearing unsupportive shoes. Athletes, pregnant individuals, and those with certain medical conditions like diabetes are particularly susceptible to this condition. The strain placed on the plantar fascia due to these factors can lead to microtears and inflammation, culminating in intense heel pain.
Pronation and Heel Pain: A Common Connection
Another significant contributor to heel pain is pronation. Pronation is the natural rolling motion of the foot that helps with shock absorption during walking and running. However, excessive pronation can lead to an uneven distribution of weight and stress on the plantar fascia, triggering inflammation and pain. Citi Footcare’s expert podiatrists can assess your gait and offer solutions to address pronation-related heel pain.
Treatment Options for Heel Pain: Your Path to Relief
At Citi Footcare, a range of treatment options is available to alleviate your heel pain and restore your quality of life. Nonsteroidal anti-inflammatory drugs (NSAIDs) can provide temporary relief by reducing inflammation and pain. In some cases, corticosteroid injections may be administered to target the inflamed area directly and offer rapid relief.
Custom Orthotics: Personalized Support for Lasting Comfort
Custom orthotics play a pivotal role in Citi Footcare’s approach to treating heel pain. These specially crafted shoe inserts are designed to provide your feet with the support and alignment they need to heal properly. By addressing the root cause of your pain, custom orthotics can significantly reduce discomfort and help you regain your mobility.
Traditional Surgery: A Tried and True Approach
For severe cases of plantar fasciitis that do not respond to conservative treatments, traditional surgery may be recommended. This involves releasing the tension in the plantar fascia by making a small incision. While effective, this approach typically involves a longer recovery period.
Minimally Invasive Surgery: Precision and Speed
Minimally invasive surgery is a cutting-edge technique offered by Citi Footcare, focusing on precision and quicker recovery. This approach involves smaller incisions and specialized instruments, resulting in less tissue damage and reduced downtime.
Shock Wave Treatment: Harnessing the Power of Sound Waves
Shock wave treatment, another groundbreaking option, utilizes focused sound waves to stimulate healing in the affected area. This non-invasive procedure enhances blood flow and tissue regeneration, offering long-term relief from heel pain.
Unlocking the City: Embrace Life Anew with Citi Footcare
Imagine strolling through Central Park, the verdant oasis in the heart of NYC, without wincing at every step. Envision yourself exploring the city’s cultural wonders, uninhibited by the constant nagging of heel pain. With Citi Footcare by your side, these dreams become your reality. It’s not just about shedding pain; it’s about embracing life in all its splendor, traversing the city’s streets with the confidence that comes from knowing your feet are in the best hands.
Why Citi Footcare Reigns Supreme in NYC
In the bustling landscape of New York City’s podiatry practices, Citi Footcare stands tall for a myriad of reasons. Dr. Emanuel Sergi’s leadership is marked by an unparalleled dedication to his craft and an unyielding commitment to his patients’ well-being. With a team of exceptional podiatrists, Citi Footcare boasts a wealth of expertise that spans the spectrum of foot care. They are relentless in their pursuit of staying up-to-date with the latest advancements in podiatric science, ensuring that you receive nothing but the best.
Embark on Your Journey to Freedom: Contact Citi Footcare Today
Don’t let heel pain dictate the course of your life. Instead, take charge and embark on a journey to reclaim your mobility and vitality. The transformation awaits at Citi Footcare, where the ultimate solution to heel pain in NYC is not a distant dream but a tangible reality. Say goodbye to discomfort, and say hello to a future where every step is a testament to your strength and resilience.
Contact Citi Footcare today:
Citi Footcare122 East 42nd Street, Ste 2901
(at 42nd and Lexington Ave)
New York, NY 10168
Phone: 212-871-0800
Email: citifootcare@gmail.com
Website: https://www.CitiFootcare.com
Revolutionary Breakthrough: Eradicate Neuroma Pain Forever with Mind-Blowing Radiofrequency Ablation!
Neuroma pain can disrupt life!
Neuroma pain is a relentless foe, capable of disrupting even the most harmonious symphony of daily life. Each step can become a painful reminder of this persistent discomfort, casting a shadow over the simplest of activities. But fear not, for a groundbreaking solution has emerged from the depths of medical innovation, a solution that promises to banish neuroma pain to the realm of distant memories: Radiofrequency Ablation. This cutting-edge technique is causing seismic ripples through the world of podiatry, and at the forefront of this seismic shift is none other than Citi Footcare, the preeminent podiatry practice nestled in the vibrant heart of New York City.

Why Citi Footcare Reigns Supreme in Neuroma Treatment in the Big Apple
Within the bustling and diverse landscape of New York City’s podiatry practices, Citi Footcare shines like a beacon of expertise and excellence. Helmed by the esteemed Dr. Emanuel Sergi, the team at Citi Footcare embodies a fusion of experience, knowledge, and a relentless commitment to advancing the field of podiatry. With an extensive and illustrious track record in tackling a wide array of foot conditions, Citi Footcare stands as an unwavering pillar of support for those seeking relief from neuroma pain.
Dr. Emanuel Sergi, along with the proficient team at Citi Footcare, has meticulously cultivated a reputation as pioneers in embracing innovative medical solutions. The journey to eradicating neuroma pain necessitates a personalized approach, a hallmark of Citi Footcare’s philosophy. By delving into the unique circumstances of each patient, the Citi Footcare team ensures that every facet of the condition is comprehensively addressed, leading not only to transient relief but sustainable and enduring results. Their dedication to patient welfare and holistic care has positioned Citi Footcare as a vanguard in the realm of neuroma treatment in the city that never sleeps.
Unveiling the Phenomenon: Radiofrequency Ablation’s Transformational Power
In the sphere of neuroma treatment, Radiofrequency Ablation emerges as a game-changer that has rewritten the rules of engagement. This groundbreaking procedure involves the strategic application of radiofrequency energy to the targeted nerve fibers responsible for the agonizing pain. The result? Swift and sustained relief, often accompanied by minimal downtime and a prompt return to normal activities.
Radiofrequency Ablation’s virtues extend far beyond the realm of conventional surgical methods. The procedure is thoughtfully designed to offer a plethora of advantages, revolutionizing the neuroma treatment landscape. With its outpatient nature, Radiofrequency Ablation liberates patients from the shackles of extended hospital stays, empowering them to reclaim their lives at an accelerated pace. The abbreviated recovery period serves as an antidote to the prolonged convalescence commonly associated with traditional surgical interventions, enabling a quicker reintegration into the vibrant rhythm of New York City life.
The Path to Neuroma Liberation: Navigating the Journey
Embarking on the transformative odyssey towards liberation from neuroma pain through Radiofrequency Ablation at Citi Footcare is a journey marked by meticulous care and precision. The voyage commences with a comprehensive evaluation, a cornerstone of Citi Footcare’s patient-centered approach. Dr. Sergi and his adept team scrutinize your medical history and specific condition, meticulously determining the viability of Radiofrequency Ablation as the optimal course of action for your unique circumstance.
Once the procedure is scheduled, the fortress of apprehension dissipates, replaced by the reassurance of Citi Footcare’s expertise. The Radiofrequency Ablation procedure, under the expert guidance of Dr. Sergi and his team, unfolds with an orchestrated symphony of skill and compassion. The procedure is characterized by minimal discomfort, and the post-procedural phase is often met with an overwhelming sense of relief, as countless patients recount a rapid attenuation of their neuroma pain.
Your Gateway to a Pain-Free Existence Begins Here
The time for liberation from the clutches of neuroma pain is now. The first stride on this transformative path involves the initiation of a dialogue with Citi Footcare, the esteemed custodians of your neuroma liberation. The unparalleled expertise of Dr. Emanuel Sergi and his proficient team awaits, poised to guide you through the formidable landscape of Radiofrequency Ablation.
Connect with Citi Footcare:
Address: 122 E 42nd Street Ste 2901, New York, NY 10168Phone: 212-871-0800
Email: citifootcare@gmail.com
Website: https://www.CitiFootcare.com
Bunion Pain: Causes, Symptoms, and Effective Podiatry Treatments in New York City
Introduction to bunions:
Are you experiencing persistent foot pain and discomfort? One common foot condition that affects many individuals is bunions. Bunions can cause significant pain and hinder daily activities. If you’re seeking relief from bunion pain in New York City, look no further than Citi Footcare. Our team of highly skilled podiatrists, led by Dr. Emanuel Sergi, specializes in providing effective treatments for bunions, ensuring you can regain your mobility and live pain-free.

What are Bunions?
Bunions are bony bumps that form at the base of the big toe. They develop when the bones in the front part of the foot move out of alignment, causing the big toe to lean inward and crowd the other toes. This misalignment creates a protrusion on the side of the foot, leading to pain, swelling, and discomfort. While the exact cause of bunions is not always clear, factors such as genetics, arthritis, and wearing ill-fitting shoes can contribute to their development.
Symptoms of Bunions:
- Visible Bump: A bony protrusion on the side of the foot near the big toe.
- Foot Discomfort: Pain and tenderness around the affected area, especially when walking or wearing tight shoes.
- Toe Misalignment: The big toe points inward and may overlap or push against the adjacent toes.
- Swelling and Inflammation: The affected area may become red, swollen, and warm to the touch.
- Corns and Calluses: Thickened skin may develop over the bunion, leading to additional discomfort.
Effective Bunion Treatments:
- Non-Surgical Options:
- Footwear Modifications: Wearing comfortable, wide-toe shoes with adequate arch support can relieve pressure on the bunion.
- Orthotic Devices: Custom shoe inserts can help distribute pressure evenly across the foot, reducing pain and preventing bunion progression.
- Padding and Taping: Applying pads or tape over the bunion can cushion the area and reduce friction.
- Medications: Over-the-counter pain relievers and anti-inflammatory drugs may alleviate pain and reduce swelling.
- Surgical Options:
- Bunionectomy: In severe cases where conservative treatments fail to provide relief, surgery may be necessary to realign the bones and remove the bunion. Our experienced podiatrists at Citi Footcare can assess your condition and recommend the most suitable surgical procedure.
Why Citi Footcare is the Best Choice for Bunion Treatment in New York City:
At Citi Footcare, we prioritize patient care and provide personalized treatment plans tailored to each individual’s needs. Our team of expert podiatrists, including Dr. Emanuel Sergi, has extensive experience in diagnosing and treating bunions. We stay up to date with the latest advancements in podiatry to offer our patients the most effective and innovative treatment options. With our commitment to excellence, compassionate approach, and state-of-the-art facility, we are proud to be the premier choice for bunion treatment in New York City.
Call today to schedule a consultation:
Don’t let bunion pain hold you back from enjoying life to the fullest. Contact Citi Footcare today to schedule a consultation with Dr. Emanuel Sergi or one of our skilled podiatrists. We will assess your condition, develop a customized treatment plan, and guide you towards a pain-free and active lifestyle.
Citi Footcare122 E 42nd St Ste 2901
New York, NY 10168
Phone: 212-871-0800
Website: https://www.CitiFootcare.com
Email: citifootcare@gmail.com
Lapidus Bunionectomy
 This patient presented to our office with a large painful bunion of the left foot. During the in office consultation we noted that the 1st metatarsal was also hyper-mobile. Hyper-mobile means that the first metatarsal moved up and down too easily with minimal pressure. Looking at the x-ray on the left you can see how much the the first metatarsal has shifted away from the second. This type of deformity does not happen over night, but may take many years to develop. We decided that a proximal osteotomy with internal fixation consisting of both screws and a plate would be the procedure of choice. The surgery was performed and we corrected the deformity utilizing a Lapidus type bunionectomy. From the x-ray you can also see that minimal shortening was achieved along the first metatarsal.
This patient presented to our office with a large painful bunion of the left foot. During the in office consultation we noted that the 1st metatarsal was also hyper-mobile. Hyper-mobile means that the first metatarsal moved up and down too easily with minimal pressure. Looking at the x-ray on the left you can see how much the the first metatarsal has shifted away from the second. This type of deformity does not happen over night, but may take many years to develop. We decided that a proximal osteotomy with internal fixation consisting of both screws and a plate would be the procedure of choice. The surgery was performed and we corrected the deformity utilizing a Lapidus type bunionectomy. From the x-ray you can also see that minimal shortening was achieved along the first metatarsal.
Recovery after bunion surgery
I’ve written a detailed description of what to expect after bunion surgery on my new site. www.bunionsurgery.nyc. This article includes what to expect immediately after bunion surgery and goes up until one year after surgery.
As I’m sure you can imagine, after 15 years of doing foot surgery, I’ve been asked lots and lots of questions about bunion surgery.
I’ve answered the following questions:
What should I expect the day of bunion surgery?
Is bunion surgery painful?
How much pain should I have after bunion surgery?
Do I take pain killers after bunion surgery?
Can I walk after bunion surgery?
What do I wear on my foot after bunion surgery?
Do I wear a surgical shoe after bunion surgery?
Do I wear a brace after bunion surgery?
How long do I have to wear a shoe or brace after bunion surgery?
Do I have a cane or crutches after bunion surgery?
How long do I keep my foot dry after bunion surgery?
How do I keep my foot dry after bunion surgery?
Do I ice my foot after bunion surgery?
Do I elevate my foot after bunion surgery?
How much walking can I do after bunion surgery?
When can I walk after bunion surgery?
How much activity can I do after bunion surgery?
How much can I walk after bunion surgery?
When can I work out after bunion surgery?
When can do the stationary bike after bunion surgery?
When can I run after bunion surgery?
How far can I run after bunion surgery?
When I can wear regular shoes after bunion surgery?
When can I wear high heels after bunion surgery?
How often should I see my doctor after bunion surgery?
When can I go back to work after bunion surgery?
Do I take antibiotics after bunion surgery?
Can I do bunion surgery on both feet at the same time?
How far apart should I do my bunion surgeries on both feet?
To see answers to all these questions click here: Recover after bunion surgery
Second Opinion for Foot Surgery in NYC
Second Opinion
Patients often come in to my office requesting a second opinion for foot surgery after they have seen another podiatrist in New York City. I always welcome my patients to seek second opinions as well.
Many times I agree with the other doctors’ recommendations for surgery. Also, many times I disagree with their recommendations. Often, I disagree because I feel they have chosen the wrong procedure for bunion surgery or hammertoe surgery.
Bunion Surgery
In regards to bunion surgery, many doctors perform distal osteotomies for large bunions that require a more proximal osteotomy. I will explain distal versus proximal osteotomies in a moment, but first let me explained why this happens. Many podiatrists are not trained or experienced in performing more difficult surgical procedures such as proximal osteotomy bunionectomies. Proximal osteotomies are much more challenging, and require much more skill than the distal osteotomies. If you have browsed this blog, you will have seen examples of large bunions that require more proximal osteotomies. This is one of my favorite topics to write about.
Small bunions can be fixed with distal osteotomies. An osteotomy is simply a medical term for a cut in a bone. A distal osteotomy is performed at the far end of the metatarsal bone just behind the toes. Most podiatrists are very experience performing this kind of osteotomy.
Larger bunions require a more proximal osteotomy. Proximal osteotomies are performed at the base of the metatarsal, further back in the foot. There are a few types of these proximal osteotomies. The most common ones are a ‘closing base wedge osteotomy’, an ‘opening base wedge osteotomy’, and a ‘scarf osteotomy’. In previous blog posts I have discussed each of these. Proximal osteotomies are much more difficult than distal osteotomies. The surgeon must be experienced and knowledgeable in order to remove the proper amount of bone, add the appropriate amount of bone graft, fixate the bone cuts properly with screws and plates, and align the bones in three dimensions.
Getting back to second opinions for surgery, I often advised patients to ask their previous doctor about their experience with these more difficult surgeries. It is not my intention to take patients away from their original doctor, but rather to inform them of my opinion on the proper surgical procedures of choice.
Hammertoe Surgery
When it comes to second opinion for hammertoe surgery, I often advised patients to have the small joints of the toes to be fused called an arthrodesis, rather than just remove part of the bone, called an arthroplasty. I perform many arthroplasty procedures but many times a joint fusion is necessary to get a better cosmetic and more permanent correction of hammertoes.
The way I fuse hammertoes is also superior in my opinion to the older methods of joint fusions. Most podiatrists use a wire that sticks out from the end of the toe in order to hold the bones together while they heal, and fuse. I prefer to use a screw that is totally within the toe and does not stick out. There are many advantages to this method. The most important in my opinion, is that the screw creates compression between the 2 bones pushing them together and achieves the goal of fusing the 2 bones together almost all the time. Using a pin in the toes simply holds the bones in one direction and does not push them together. The bones are free to move longitudinally in the direction of the pin as well as rotate on the pin. The screw prevents this. Additionally, the screw is buried within the toe does not stick out which allows the patient to get the foot wet in the shower after just 12 days, rather than keeping it dry for 4 weeks while the pin sticks out from the end of the toe.
I have tried many of the new implants that have been designed for hammertoe fusion. These are very extensive pieces of metal that go inside the toe in order to avoid the need for the pin to stick out from the end of the toe for 4 weeks. Unfortunately, I have not been satisfied with any of them. They all fail to have one importance quality that the screw has. Only the screw pushes the two bones together called compression. These new implants hold the bone in 2 directions. They stopped the bones from rotating and moving up and down, but all fail to push the bones together in that third longitudinal direction that I think is necessary in order to increase the chances that the bone will heal together.
A Story about Second Opinion for Foot Surgery
Now that I have discussed second opinions for bunion surgery and second opinion for hammertoe surgery, let me tell you a story about second opinions for surgery.
Unfortunately, there are some unethical doctors that consider monetary gain as a reason to do surgery on patients. In the past few weeks, I have seen three patients that came to me for second opinions for foot surgery that I told not to have surgery. It is unfortunate and disturbing that these doctors recommended surgery when it was not necessary or recommended the wrong procedure.
Interestingly, two of the patients came from the same unethical doctor. This doctor recommended surgery for a 15-year-old patient with plantar fasciitis without performing any conservative care. First of all, the patient was only 15 years old and not done growing completely. Secondly, I would estimate 98% of patients with plantar fasciitis do not need surgery, and get better with conservative treatment. There are many treatments for plantar fasciitis that do not involve invasive surgery. In fact, there are at least 10 different treatments that are regularly done before surgery is recommended. This doctor only recommended one treatment, custom molded orthotics. I speculate that this treatment was recommended because orthotics can be profitable for the doctor. Orthotics alone are not the recommended treatment for plantar fasciitis. They are a good long-term solution to prevent it from returning as well as helping other acute treatments. I told this 15-year-old patient and his parents that he should not have surgery until all conservative measures are exhausted.
The next patient that came to me for a second opinion for surgery from the same unethical doctor that they saw previously had a soft tissue mass on the top of her foot. The mass had been there for only a few weeks. The patient had no associated pain and it was very small, and not a cosmetic concern. The previous doctor did an ultrasound in his office on the first visit and told the patient that he did not like the looks of the lesion and scared her that it may be cancerous. He recommended surgery as soon as possible to remove the soft tissue mass. She came to me for a second opinion for foot surgery to remove the soft tissue mass. I also did an ultrasound in my office that showed the mass was a simple fluid-filled ganglion along one of the tendons. Treatment for a ganglion involves aspiration of the fluid out of it and injection of steroid to prevent it from coming back. I would only recommend surgery if, and only if, this treatment failed two to three times to get rid of it, and it was also symptomatic/painful or a major cosmetic concern. Additionally, if I had suspected anything more than a simple benign lesion I would order an MRI to evaluate it prior to surgery.
The next patient that came to me for a second opinion involved her toenails. Her doctor had removed 9 of her toenails in order to treat nail fungus. When the nails grew back exactly the same as they were, he recommended repeating the procedure. She came to me for a second opinion on nail removal. When I examined her I concluded that the discoloration and thickening of her toenails was not due to fungus. It was due to repetitive trauma from tight shoes that damaged the nail roots. To be sure, I sent a sample of the nail to the laboratory for biopsy for a pathologist to look under the microscope for fungal elements. As I suspected, the biopsy came back negative. Had the biopsy been positive, treatment would still not have been surgical removal of the nails. Fungal nails are much better treated with laser or oral medication, as removal of the nails rarely works. It is sometimes painful and can sometimes cause damage to the nails that is permanent. When there is damage to the nail root surgical removal of the nail rarely works also to resolve the discoloration and thickening. Most of the time, the nail grows back exactly the same or can be worse. Sometimes I will remove nails but I informed patient that there is a greater chance that they will grow back the same. If it is one or two nails, I am more likely to perform this procedure than when many more are affected.
Besides these unethical behaviors most patients come in for second opinions when surgery is indicated. I give my honest opinion as to what procedures I recommend and inform the patient of risks, complications and postoperative expectations. I do not ask the patient who the previous doctor was until the end of the visit and reserve any judgment about the doctor as that is ethical behavior.
So, if you require a second opinion for foot surgery, please call and schedule a consultation.
Bunion Surgery Done the Right Way
Case of the day:
Bunion surgery for a large bunion
Four weeks ago I performed bunion surgery on a patient with a very large bunion. She came in today for her four week follow-up visit.
She had a large bunion with constant pain in her great toe joint.
Bunion surgery for a large bunion, before and after pictures.


Before and after large bunion surgery x-rays


I performed two procedures:
Scarf bunionectomy
A scarf bunionectomy cuts the metatarsal bone down the center allowing me to rotate half of the metatarsal toward the other toes to straighten the angles.
Akin bunionectomy
An akin bunionectomy cuts the first toe bone and removes a wedge allowing me to move the big toe back the other way, away from the other toes in order to straighten it.
For large bunions you can’t just do a ‘distal osteotomy’ as most doctors do.
If you suffer from a large bunion, contact my office to schedule a surgical consultation.
Dr. Sergi
Case Study: A large bunion with overlapping second toe
Today I would like to share with you a surgery that I performed six months ago. This patient came in today for her 6 month follow up visit. She said she was doing great, running, yoga and wearing high heeled shoes at times.
Large Bunion
This patient is a 65 year old professional. She came into my office with a complaint of pain in her great toe joint and second digit hammertoe. She had pain with exercise and could not wear feminine shoes. She said that she would like to be able to wear high heels with her business suits as she works at a big NYC bank and needs to look good for work. She also wanted to be able to exercise without pain.
Her preoperative photos and x-rays are below:
You can see that she has a large, dramatic bunion with the second toe overlapping the great toe.





I performed four procedures to correct for her bunion, hammertoe and dorsally dislocated second toe joint.
1) I performed a scarf osteotomy of the first metatarsal. I love the scarf osteotomy. It allows me to get a huge correction of the first metatarsal while allowing the patient to partially bear weight immediately postoperatively. I often do ‘opening base wedge osteotomies’ and ‘closing base wedge osteotomies’ but they require the patient to be on crutches for 10-12 weeks. The scarf osteotomy is one of the most challenging procedures to perform but I do a lot of them and have mastered this difficult procedure. The base wedge osteotomies allow for more correction than the scarf so some patients with large bunions will still need to use crutches when I do them.
2) I next performed an ‘akin osteotomy’ of the great toe, proximal phalanx. If you can imagine that the toe is connected to the metatarsal bone when the metatarsal is moved toward the second toe, the great toe goes with it. I then move the great toe back the other direction by adjusting the soft tissue holding it. When I cannot get the great toe to be parallel to the second and it still leans toward the second toe, I then cut the great toe bone and take out a small wedge to move it away from the second toe.
3) I next performed a lengthening procedure of the tendon and other soft tissues holding the second toe upwards.
4) I next performed a fusion of the bones in the second toe to keep it straight forever. I like to fuse toes with screws rather than pins or other fusion implants. I find that the screw holds the toe straightest and I am able to compress the two bones together. This allows for the highest success rate of getting those two bones to heal together. Another advantage of using screws over pins is that the pin needs to stick out through the skin. This allows for a higher chance of getting an infection and the patient needs to keep their foot dry for four weeks versus 12 days with the screws. I then take the screw out with a small surgical procedure under local anesthesia anywhere from 6 weeks to 6 months after it is put in depending on the patient. This is one of the only times I remove screws postoperatively.
The below x-ray was taken three months postoperatively. You can see healing of the bones, especially the fusion of the second toe bones next to and around the screw.
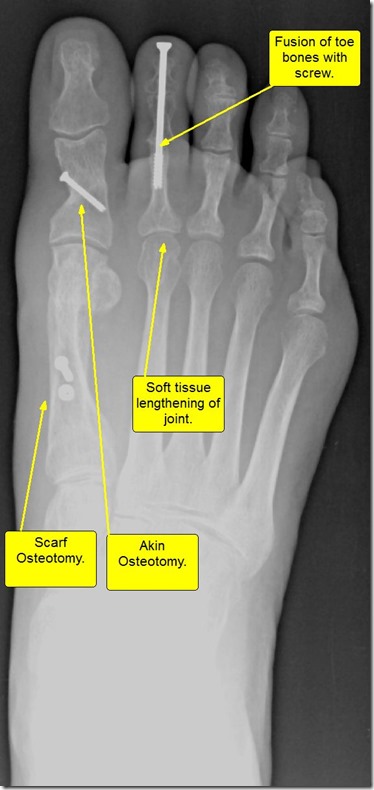

Below are before and after pictures of this surgery for a large bunion with overlapping second toe.
Please note also that these after surgery pictures were taken at only six months. It takes up to a full year for the scar tissue to go down and the foot to look less ‘fat’, and for the scars to mature completely. I’ll post pictures again in an additional six months.









I enjoy treating the most challenging problems but also enjoy the more ‘regular’ surgeries.
I hope you enjoyed reading about this challenging bunion surgery as much as I enjoyed writing about it and presenting it you.
Emanuel Sergi, DPM
Pain in the big toe joint. Hallux Limitus Surgery including before and after pictures. Arthritis of big toe joint.
Hallux Limitus Surgery
This pain can be caused by many things. I’ve already written blog articles on bunions and gout which are two very common causes of great toe joint pain. Click these links for those articles. Gout. Bunions.
 The medical term for the big toe joint is the “first metatarsal phalangeal joint”. This is because the two bones that make up the joint are the “first metatarsal bone” and the “first proximal phalanx bone”. (Click any picture to enlarge). Doctors often refer to the big toe joint (“First Metatarsal Phalangeal Joint”) as the “First MPJ” or just “MPJ”.
The medical term for the big toe joint is the “first metatarsal phalangeal joint”. This is because the two bones that make up the joint are the “first metatarsal bone” and the “first proximal phalanx bone”. (Click any picture to enlarge). Doctors often refer to the big toe joint (“First Metatarsal Phalangeal Joint”) as the “First MPJ” or just “MPJ”.
Pain in the big toe joint is one of the most common complaints I hear in my podiatric surgery practice.
I really enjoy doing surgery for MPJ pain caused by arthritis in this joint because the surgery works so well. Arthritis is a general term for pain and inflammation of a joint and can be used to refer to any joint in the body.
Arthritis of the big toe joint can be caused by many things: bunions, gout, inflammatory arthropathy such as rheumatoid arthritis and other autoimmune diseases, trauma, infection, bad shoes, overuse such as athletes, congenital malformation, congenital anomalies such as longer or shorter bones than normal, higher or lower bones than normal, misshaped bones or cartilage, functional anomalies like flat feet or curvature of bones of the leg, and some other that I’m sure I left out of this list.
Most of the above lead to the slow progression of arthritis in the form of loss of cartilage of the joint. Cartilage is the smooth semi-hard substance between bones that allows bones to glide smoothly together in a joint and not grind or scrape each other. Once the cartilage is gone, bones grind on one another and cause pain and decreased range of motions.
 Additional sequelae of arthritis is formation of bone spurs. Bone spurs usually grow due to small micro-trauma to the bone that heals by producing more bone. Each time the bone heals the tiny breaks, it produces more and more bone until finally you have a piece of bone sticking out where it should not be. Bone spurs can cause joint to not move by blocking the normal range of motion.
Additional sequelae of arthritis is formation of bone spurs. Bone spurs usually grow due to small micro-trauma to the bone that heals by producing more bone. Each time the bone heals the tiny breaks, it produces more and more bone until finally you have a piece of bone sticking out where it should not be. Bone spurs can cause joint to not move by blocking the normal range of motion.
Once a joint doesn’t move, your body compensates by trying to move other joints to make up for the lack of motion. This, in turn, causes those other joints to have abnormal forces and range of motion and they get overused and injured leading to arthritis.
Signs and symptoms of big toe joint arthritis.
Arthritis of the big toe joint presents with pain in the joint that usually starts off minor and intermittent and slowly progresses to happen more often and with more intense pain. Activities or certain shoes that didn’t hurt in the past, start to hurt more often and more intensely. Women often tell me that they progressively can wear their high heel shoes for less time or less distances before the pain starts. They say that they have to wear lower heels than previously. Patients report they cannot exercise as much as they used to before having pain. Arthritis is a problem that slowly progresses as the cartilage wears away.
Sometimes people have arthritis but do not know it. I wrote an article not too long about about people who have bunions but no pain associated with them. One of the only times I tell people to have bunion surgery when they are not in pain is when they have signs of arthritis on x-ray but no associated arthritic pain. See the article here: When to have bunion surgery when you do not have pain.
One of the main reasons people come in to see me for big toe joint pain is for something called Hallux Limitus. This Latin term comes from the word Hallux which is the medical term for the big toe and Limitus, which means limited range of motion of a joint.
 Hallux Limitus can be broken down into two major categories but both describe lack of range of motion of the big toe joint. The first kind is called Structural Hallux Limitus. This describes a joint that cannot move enough due to changes in the structure of the joint. This can be due to lack of cartilage between the bones, bone spurs that block the motion and sometimes bone growth that actually fuses the bones together. When the bones fuse together two bones actually become one piece without any space between them.
Hallux Limitus can be broken down into two major categories but both describe lack of range of motion of the big toe joint. The first kind is called Structural Hallux Limitus. This describes a joint that cannot move enough due to changes in the structure of the joint. This can be due to lack of cartilage between the bones, bone spurs that block the motion and sometimes bone growth that actually fuses the bones together. When the bones fuse together two bones actually become one piece without any space between them.
The second kind of hallux limitus is called Functional Hallux Limitus. This describes a condition in which the bones don’t move enough due to abnormal forces on the bones of the foot. Most commonly people who have arches that collapse or flat feet have functional hallux limitus. When the arch collapses the first metatarsal bone gets pushed up and out of the way by the ground forces. When the first metatarsal is elevated, the phalanx bone cannot move up enough to make it over the metatarsal and flex upwards to bend the toe joint.
Functional hallux limitus leads to arthritis and bunions. In my article and video about bunions I describe how functional hallux limitus causes the bunion. See those articles and videos by clicking the links at the end of this paragraph. This blog will focus on hallux limitus and joint arthritis. Video describing bunions. Article describing bunion formation.
As I stated above, functional hallux limitus often leads to big toe joint arthritis by causing abnormal forces on the joint and wearing away of cartilage which in turn leads to structural hallux limitus with loss of cartilage and bone spurs that block motion.
Okay, we’ve now discussed what causes hallux limitus and arthritis as well as signs and symptoms of big toe joint arthritis. Next we will discuss treatment and surgery of them.
When a patient comes into my office with a complaint of big toe joint pain, I first do a thorough history and physical exam. I ask them all about the pain including what it feels like, where they get it, how long have they had it, what was the onset like, fast or slow progression, what activities cause pain, what shoe types cause pain, and what treatments have they tried and which worked or did not work.
Once I’ve established that detailed history I start my exam. I check the entire foot starting with the circulation, the nerves, and the range of motion of all the joints including the big toe joint. I check the muscle strength and tendons. I have the patient stand up to see how the foot looks weight bearing.
The next part of the examination is the x-rays. The x-rays tell a big part of the story. I look for the length and position of the bones. I look at the amount of cartilage of the joints. I look for bone spurs or bone cysts. I look at the overall bone structure of the foot.
Once I’ve completed my history and exam with x-rays I am able to determine the extent of the problem and the cause(s) of it. I then explain to my patients in layman’s terms all of this info.
The next and most important step is the treatment of big to joint pain and arthritis. Most often the treatment is surgical but there are a few non-surgical treatments that can be done.
I take great pride in my ethics and the ethical treatment of my patients that trust me to take care of them. I will try to keep this tangent as short as possible but I’m very passionate about the subject. I have a tremendous respect for my patients. I feel privilege to be a doctor and take care of patients. Strangers come to me for help and expect me to do the right thing, tell them the whole truth, and act in their best interest, not my own. I often think about other circumstances in life where this happens and I, unfortunately, cannot think of many or any for that matter. It seems that all businesses out there are out for profit and not for altruism.
I make most of my profits by performing surgeries but I would never tell a patient that they need surgery when I can help them with a less invasive, less risky, less painful alternative non-surgical treatment. Unfortunately, in my career I have come across many doctors that do not practice this way and do make decisions based on profit to some extent at the cost of their patients but I will not expand on this further here.
Okay, sorry about that divergence, back to treatment of big toe joint pain. I was about to tell you about the non-surgical treatment of big toe joint pain. When the arthritis is not too severe non-surgical treatment works better than once the arthritis has progressed more. When there is functional hallux limitus and not structural hallux limitus, as described above, non-surgical treatment works better.
Non-surgical treatment includes two things. The first is what we call palliative care. This means treating the symptoms of the problem, not the cause of the problem. The symptoms are pain and inflammation. We treat pain and inflammation with anti-inflammatory medications, or pain killers; pills and injections. Pills are often non-steroidal anti-inflammatories such as aspirin, Motrin, Aleve, Celebrex and many over-the-counter and prescription medications. Sometimes we use steroid pills as well for more severe inflammation. We also treat inflammatory symptoms with icing, rest, compression and physical therapy modalities.
The second kind of non-surgical treatment addresses the lack of motion of the joint. We can increase range of motion with physical therapy and custom foot orthotics. Again, these work better for functional hallux limitus and not structural. Structural hallux limitus almost always requires surgery.
As stated earlier, I like performing surgery for hallux limitus. The reason I like it is because by the time people need surgery they are usually in a great deal of pain and it affects their lifestyle, and it is such a big relief for them when I correct the problem.
After I evaluate the cause and extent of the problem I decide on which surgical procedure to perform. There are a few different procedures to choose from. I’ll list them here and then describe each one. These procedures include: Cheilectomy, decompressional metatarsal osteotomy, Keller procedure of the proximal phalanx, joint implant arthroplasty, and joint fusion.
Cheilectomy procedure for hallux limitus.
The least destructive to the joint is called the Cheilectomy. A cheilectomy involves simply cleaning up the joint. I remove bone spurs and loose extra bones in order to allow the joint to move more freely and more normally. When I choose this procedure the cartilage has to be mostly intact as it does not address the lack of space between the bones, but only the extra bones that block motion.
Below are before and after pictures of Cheilectomy procedure. Click to enlarge.
Decompressional Osteotomy, Youngswick procedure for hallux limitus.
One of the most common procedures I do is the decompressional metatarsal osteotomy procedure. One of these is called the Youngswick procedure named after the doctor that first described it. This involves cutting the metatarsal bone and moving it down and back in order to create more space between the metatarsal and the proximal phalanx. This is used to address a long or high metatarsal or a functional hallux limitus. Again, this procedure often requires there to be some cartilage left on the bones. Recently, I have been modifying this procedure in my own unique way in order to treat more advance loss of cartilage and I’m having excellent outcomes.
Below are before and after pictures of a decompressional osteotomy. Click to enlarge.
Keller Procedure for Hallux Limitus:
The next procedure is called the Keller procedure. This procedure is called more joint destructive because it involves removing part of the joint. I remove the base of the proximal phalanx bone in order to create a space between the bones. The trick here is to maintain that space for years after the surgery as it has a natural tendency for the bones to move back together over time. There are many ways doctors try to maintain this space including using metal pins to hold the bones while they heal, implanting cadaver soft tissue grafts and skin components between the bones and various other ways. I feel my way is the best and I have seen patients follow-up long term with preservation of the space. I modify the joint capsule around the joint and use it as a spacer between the bones. This is the most challenging and difficult part of the procedure but I have discovered a way to make it work.
Below are before and after pictures of a Keller Procedure. Click to enlarge.
Implant Arthroplasty for Hallux Limitus:
The next procedure is the great toe implant arthroplasty or great toe joint implant procedure. I have performed many of these procedures in the past but often prefer other procedures over them. They work very well to reduce the painful arthritis but they often get stiff over time. This procedure involves removing either the head of the metatarsal or the base of the proximal phalanx and replacing it with a metallic joint implant. The advantages are that it maintains the length of the toe cosmetically. The disadvantage is that I find they get stiff over time. I have not done one of these procedures in a while because many patients reported stiffness postoperatively.
Below is a picture of after a joint implant Procedure. Click to enlarge.
Joint fusion or metatarsal phalangeal joint arthrodesis for hallux limitus.
The last procedure is called the joint fusion. This involves permanently fusing the metatarsal and phalanx bone together. The theory here is that if there is no motion, there is no pain, and that theory almost always works. The disadvantage is that you never can move your big toe joint again. This means that women can never wear a high heel again. Also, it can slow a patient down because as we walk faster or run, we need the big toe joint to move up more and the fusion blocks that. I reserve the fusion for patients that are more sedentary. I often perform fusions for people that have major angular deformity of the bone as well. When there is contracture of the soft tissues that misaligns the big toe joint or when the bones have been previously altered in other surgeries, I will perform a fusion.
In the below example, I felt there was just no way that any less invasive procedure would realign this joint and give satisfaction to the patient. She had previous bunion surgery by another surgeon that had a bad outcome. In the end I fused her joint and her pain completely went away. She fit into shoes that she had not previously. She was an older patient that did not need to the mobility of a younger patient. She was extremely happy with the result and was pain free last I spoke to her over a year after surgery.
Below are before and after pictures of a joint fusion Procedure. Click to enlarge.
As you can see I am passionate about big toe joint pain and consider myself an expert in it. I hope you enjoyed reading this article as much as I enjoyed writing it. As with most of my articles I expect thousands of views from people around the world. I always love comments and emails about my articles and encourage them. I wish I had enough time to write back to everyone but it has gotten a bit overwhelming to do so. I will try to write back to some of you time permitting.
Dr. Silverberg quoted for NBC’s Today Show on: Pregnancy Foot Problems.
I’m pleased to announce I was asked to contribute to a story on NBC’s Today Show (Moms Section ![]() ) on High Heels and Pregnancy.
) on High Heels and Pregnancy.
Pregnancy Foot Problems
I was asked about foot problems women face during pregnancy and my opinion on wearing high heels during pregnancy.
Click the below picture to go to the article.

Bunion Surgery Including before and after pictures of bunion surgery.
Updated 2013 03-03
Originally posted 2010 11-18
Bunion surgery is the most common foot surgery I do. Before I tell you about the actual surgery, I will describe what a bunion is and how a patient gets one. Below is a picture of a severe bunion deformity and a moderate to minor bunion. See further below for before and after bunion surgery pictures. (Click any picture to enlarge)
Bunions are also called “hallux abducto-valgus” in medical terms. Hallux refers to the great toe. Abducto-valgus refers to position of the great toe such that it points towards the other, lesser toes and is rotated. The bunion deformity consists of the movement of two bones at the great toe joint. The further back bone, called the first metatarsal, moves toward the midline of the body and the toe bone, called the proximal phalanx, moves in the opposite direction toward the other toes.
Bunions are mostly genetic. Very rarely, people are born with a bunion deformity called a juvenile bunion, but almost all bunions occur later in life due to forces on the foot. People who have arches that collapse or feet that flatten out get bunions. In that sense, people are born with the genetic predisposition to get bunions later in life rather than being born with a large bump sticking out of the side of the foot.
People who get bunions have many different foot types. Some people have no arch when they’re standing or sitting. Other people have a normal arch that collapses to a flat arch. Even people with high arches that collapse to a more normal arch can get bunions.
When the arch of the foot collapses, the force of the foot on the ground causes the great toe to decrease in its range of motion. This is called “functional hallux limitus”. This simply means that the great toe cannot move through its normal range of motion as you push off the ground. Obviously when you push off, the toe needs to move somewhere. When the great toe cannot move straight up, the foot turns more to the side and you roll off the inside of the foot and great toe. This creates a force pushing the toe toward the other toes. Slowly over time the great toe gets pushed toward the other toes which in turn, pushes the metatarsal in the opposite direction.
Symptoms of bunions: Some people can live with bunions for their entire life without having any pain. Many people experience pain with pressure from shoes due to the metatarsal bone sticking out. Other people experience severe pain in the joint with any range of motion. Many people report that they cannot find shoes to fit. Often people also report that their exercise and activity is limited due to the pain.
Below is a picture of an x-ray of a foot with a bunion inside of a shoe. It clearly shows how a foot with a bunion fits in a shoe. This is a male patient. As you can imagine, Men’s shoes are much more forgiving than womens’. Notice how the shoe is the proper size / length but the foot is too wide for the shoe. Not only does it put pressure on the great toe joint but also on the other side of the foot at the 5th toe.
Cosmetics: Often people come into my office and report that aesthetics alone are the reason that they seek treatment for bunions. Many request that I perform cosmetic foot surgery for bunions. I often perform bunion surgery for cosmetic reasons alone, however, as an ethical physician, I have a lengthy discussion about this with patients: I describe to my patients that when a person comes in with a painful bunion and says they have a 6 or a 7/10 pain scale for example, I can do bunion surgery to make the foot look very nice and they may end up with a pain that is a 0 to 1/10. These people are very happy as their pain is significantly reduced and the foot looks much better. When a person comes in with a cosmetic complaint only about the bunion and a 0/10 on a pain scale, I warn them that they may have an occasional minor 1/10 pain after surgery. While there is a small chance of this, this is a concern. Due to the unique function of the foot in weight bearing, it is different than other cosmetic surgeries. In my experience, about fifty percent of these people proceed with the bunion surgery and fifty percent thank me for being honest and put it off for the future if and when they have pain.
Conservative treatment of bunions: Unfortunately, there are not many options for conservative treatment for bunions. If caught early, orthotics (insoles in your shoes) can alleviate some of the forces that cause the bunions. While this will not remove the bump on the foot, it will slow down or stop the progression of the bunion due to the forces I described above. Other conservative treatment for bunions address the pain due to the deformity. This includes changing shoes in order to accommodate for the large bump, anti-inflammatories, icing, padding and shielding, cortisone-type injections into the joint, and occasionally physical therapy.
Surgical treatment of bunions: I advised the patient that surgical treatment for bunions is necessary when the patient has pain that limits their ambulation, activity level and if they cannot wear the shoes they would like to wear. Surgery for bunions is elective. The patient chooses if and when they do it. Note: elective surgery is not the same as cosmetic surgery. Elective surgery is covered by insurance, cosmetic surgery is not.
The bunion surgery is done as outpatient surgery meaning that patients do not stay overnight. The surgery is done either in a hospital or an outpatient surgery facility. An anesthesia doctor (anesthesiologist) Will give the patient an IV. The procedure is done under sedation. This means that patients will be asleep, however, they will be breathing on their own. This is not general anesthesia which requires a tube down the throat to assist in breathing. Patients are required to have an adult pick them up from the surgery to ensure they get home safely after the anesthesia.
The type of bunion procedure I choose depends on how severe the bunion is. It ranges from simply shaving off a bump of bone, to cutting and moving bones, removing pieces of bone, joint implants, and occasionally joint fusions. The procedure normally takes me approximately 45 minutes to one hour to do. I make an incision on the side of the foot so that the scar is not visible. Some doctors put the scar on top of the foot; however, I feel there is no need to have a visible scar. Once inside, I access the bone and remove a small piece. I then make a cut in the bone and move the bone back where it belongs. I usually use a small titanium screw to hold the bone in place for healing. I then do any soft tissue rebalancing of the joint that is necessary. I also perform skin-plasty procedures to remove the excess skin that has formed over the bunion over time. This is a cosmetic addition to fixing bunions. The goal is improving the feel and aesthetics of the foot. I then close the skin with a plastic surgery type stitch that is underneath the skin surface so that it scars less. Having trained with plastic surgeons during my residency, I perform a more cosmetic bunion surgery than almost all other surgeons. (For more information about this see my procedures page of my website by clicking here!)
What to expect after bunion surgery: I almost always perform bunion surgery on Fridays. This allows the weekend for resting. I instruct patients that they must remain at home for Friday, Saturday and Sunday. (Walking to the bathroom and kitchen only). People that have desk jobs may do the surgery on a Friday and return to work on Monday, however, if they can take one week off of work I recommended it. People that have jobs that require them to be on their feet all of the time, I advised to take three to four weeks off of work. After the surgery patients will wear a surgical shoe or fracture brace for four weeks. Some patient have no pain at all and some patients have a lot of pain. Most people have moderate pain that is well controlled with the pain medicine that I prescribe. Note: there are surgical techniques that I employ that reduce the amount of postoperative pain. I also prescribe five days of antibiotics after the surgery to prevent infection. Patients must keep the foot dry for 10 days. I dispense a shower bag before the surgery. I will see patients once a week after the surgery until I feel that they are stable to start skipping weeks. I usually do the first visit on the Wednesday after the Friday of surgery. At this time I inspect the foot to make sure there are no problems. I will take an x-ray and usually wrap the foot in a soft cast. They return the following Wednesday, 10 days after surgery. At this time I usually let them get their feet wet and rewrap the foot themselves.
After spending four weeks in the surgical shoe or the fracture brace I allow patients to start wearing loose-fitting shoes or open shoes in the warmer weather. At this time they may start to increase their walking a bit. I advise them that they will most likely not be doing exercise until six to eight weeks after surgery. Initial exercise includes walking and using a stationary bike. After eight to ten weeks they may start to do an elliptical machine or more weight bearing exercises. At eight weeks, I advise them that they may start using any shoe that they fit into.
Below are just a couple of examples of before and after pictures of bunion surgery.
Bunion Surgery Before and After
The first example of before and after pictures of bunion surgery are of a severe bunion. The after picture is at only three months.
This patient’s x-rays are show below before and after bunion surgery.
Below: Another bunion surgery before and after pictures. The after pictures are 4 years after surgery. This patient had both of her feet done.
Left: (Below)
Right: (below)
The next patient had bunion and tailor’s bunion surgery. Fifth metatarsal osteotomy and first metatarsal osteotomy procedures. The after picture is immediate, still on the operating table. Note: the discoloration of the foot is due to the Iodine and the fact that the tourniquet is still inflated. I use a tourniquet (like a blood pressure cuff around the ankle) to stop the bleeding so I can see better while operating. (Below)
I hope you found my post on bunion surgery informative. If you have any questions please feel free to post a comment or email me, Dr. Sergi. Please also see www.cityfootcare/procedures
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd St Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.
A metaphor of how insurance companies and doctors interact. A great explanation for the layperson.
I did not write the article below in this blog post. I read this article from 2009 and was so impressed I decided to repost it here. I loved how it explains what physicians go through with insurance companies.
A great explanation about insurance companies for the layperson.
Physicians are really interested in provided excellent health care while covering our very high overhead for business and making some profit at the same time. Everyone goes to work to make money, including doctors. Speaking for myself, and I’m sure most of my colleagues, we feel as though we should be compensated well for providing such a necessary service, taking care of illness and injury, our years of higher education and post-graduate training, and the high cost of malpractice insurance with the added risk of being sued by malpractice attorneys.
The insurance companies, on the other hand, are only about making profits for their shareholders and officers. Their share price does not reflect the health care provided to their customers, only how much profit they can report.
In my 13 years of practice I’ve seen the situation get worse and worse with insurance companies paying less and less, and patients out of pocket expenses going up more and more. Add that to the annual increase in insurance premiums paid by patients and their employers and it creates negative emotions. I hear all the time from patients complaining that their insurance premiums have gone up and their responsibilities to pay the doctors have also gone up.
I have had to hire additional employees just to try to get paid from insurance companies because they deny more and more claims all the time. My accounts receivable is the biggest it has every been. We are constantly fighting to get paid. Patients get seen and we often do not get reimbursed from the insurance companies, only partially reimbursed, or paid months after the service was provided. Patients do not appreciate getting billed at all for services when they pay so much money for insurance, and also don’t understand why we bill them many months later after we are done fighting with the insurances and the claims were denied.
The below article is a great metaphor of how this third party payer system works from the providers point of view. Enjoy…
How do doctors get paid?
Imagine going to your favorite restaurant. You are greeted at the door by the hostess, who seats you and takes your drink order. You order through your favorite waiter, Andrew, who recommends the special of the day: prime rib with a dinner salad and a chocolate torte for dessert. Soon after, the food is brought out and it is delicious! You have time to enjoy your food. You then receive the bill and pay for your meal, returning to your home satisfied, all your dining needs met. Let’s say, for simplicity’s sake, you paid $75 for this meal: $50 for the steak, $10 for the salad and $15 for the dessert.
A change then occurs in the restaurant industry. A new form of eating out has been adopted. Your favorite restaurant has now contracted with over 30 different ”restaurant insurance companies.”
Anticipating another pleasant dining experience, your return to the restaurant with your new “subscribers card.” You pay your $5 “copay.” You sit in the foyer of the restaurant. You wait an hour, even though you made reservations. A harried Andrew greets you and quickly takes your order after you briefly glance at the menu. The food arrives at your table. As you take your second bite, Andrew informs you that “your time is up” and the table is reserved for another party. You are escorted outside with your hastily boxed left-overs.
What has happened to the restaurant? Behind the scenes, the restaurant owner has learned some tough realities of the “new system.” During the first month of taking insurance, the owner sends a form to the insurance company requesting payment for the $75 steak dinner: $50 for the steak, $10 for the salad and $15 for the torte. The contract with the insurance company already states that they will only pay $45 for the $50 steak, but the owner decides that the extra customers brought to the restaurant by contracting with this insurance company will more than off-set this small loss.
The first attempt at collecting the $75 dollars for the full meal is returned unpaid with the note that it was rejected due to a “coding error.” The forms for payment from the insurance company require the owner to list the parts of the meal, not by name, but by the numerical codes. The owner had listed the salad by the wrong numerical code. No suggestions for the correct code are offered, so the restaurant owner purchases a series of books, at a cost of $500, to learn how to assign the correct code to the different parts of the meals. These books will need to be bought annually due to the constant changing of the code numbers. After 30 minutes of study, the owner realizes the dinner salad should be coded as a 723.13, not the723.1 the owner originally put on the form. The salad, it turns out, needed to have two digits after the decimal point, indicating that it was a dinner salad, and not a “main course” salad. The owner mails the corrected form.
In response to the second request for payment, the insurance company does not send a check, but a detailed questionnaire: Was garlic used in seasoning the steak? Was it necessary to use garlic for this particular recipe? Did the restaurant ask for permission to use garlic from the insurance company before serving the steak? Why was salt, a less expensive alternative, not used instead? The owner submits the answers, emphasizing that the garlic is part of a secret family recipe that made the restaurant famous.
The owner waits another week (it has now been 3 weeks since the dinner was served). The check arrives three and a half weeks after the meal was served. The check is for $20 and states that it is specifically for the steak. The check also comes with a letter stating that no billing of the patron may occur for the salad, but no other explanation is enclosed. No mention is made of the $15 dessert.
The now frustrated restaurant owner calls the provider service number listed in the contract. After five separate phone calls to five different numbers (The harried voice behind phone call number four explains that the insurance company has merged with another insurance company and the phone numbers had all changed last week, sorry for the inconvenience…), the owner gets to ask why, when the contract says the steak will be paid at $45, has the check only been written for $20? And what happened to the payment for the $10 salad and the $15 dessert?
As it turns out, this particular patron’s insurance contract only pays $45 when the patron has reached their deductible, which this patron has not at this time. The remaining portion of payment for the steak must now be billed by the restaurant to the patron directly.
The $10 for the salad would have been paid if the patron had ordered it on a different day, but, per page 35 in the contract, because it was billed on the same day as the steak, it is considered to be part of the payment for the steak and no extra money can be collected from the patron or the insurance company.
The dessert, the owner learns, should have had a “modifier” number put with its particular billing code when billed with the steak and the salad.
Realizing that the insurance billing is quite a bit harder than anticipated, the restaurant owner hires a company, who is paid 5% of any money collected to specifically make sure these coding errors do not occur again and follow up on payment rejections. For an additional $99 per month, the billing company will “scrub” the forms submitted for payment to make sure specific clerical errors will not cause future delays in payment.
The owner now must lay off the hostess and the bus boy to pay the billing company, so these duties are now added to the waiter’s other responsibilities.
In the meantime, the restaurant owner has also had the waiter take on the job of answering the phones due to the now high volume of phone calls from patrons questioning why they are receiving bills for meals they ate over two months ago, and why did their insurance company not pay for this portion of the meal? This extra work is now resulting in longer times patrons must wait to be seated, and grumblings from the waiters who “were not hired or trained to do this kind of work.”
The owner now realizes that, although the dinner originally cost $75 to make, only $25 has been paid. The remaining $30 billed to the patron is now in its third mailing, with the first two requests for payment going unanswered by the patron. The restaurant owner realizes a collection agency must be employed in order to have any hope of receiving any portion of payment from the patron.
Each meal served now costs at least an additional $20 due to the added overhead of the billing company, coding books, and the collection agency. These added expenses have nothing to do with cooking food or providing any direct service to the restaurant’s customers.
Service to the restaurant’s patrons has been compromised with these changes as well. The owner has now over-extended the waiter, who was an excellent waiter, but is now taking on the roles of host, phone answering and table bussing.
In order to even meet the costs of providing fine dining, the restaurant owner now must seat twice as many patrons in the same amount of time.
What was once an outstanding business that focused on fine dining and customer service has now been turned into a business in the business of trying to get paid.
Alas, I wish this were a fictional tale, but it is not. The only fictional portion is that this is not your favorite restaurant, but your favorite doctor’s office, which is responsible not for meeting your dining needs, but those of your health.
Megan Lewis, M.D.
A family physician in rural Colorado.
Practice Focus:
Effective January 1, 2013, I have changed the focus of my practice. I have explained it completely in the below letter I wrote.
Summary: I will still see new patients but I will focus on Podiatric Surgery. When new patients do not require surgery they will follow up with my partner doctors after I have diagnosed them and made a preliminary treatment plan. I will continue to oversee their care when necessary.
To my valued patients:
As 2012 comes to an end, I am humbled and proud to acknowledge, and share with you, that my first twelve and a half years in practice have been successful beyond my predictions! After finishing residency, I moved to New York City in 2000 with a job only one half of one day per week. I quickly made valuable connections and filled my week with office hours and patients in four New York City Boroughs and Westchester County. Within two years I had opened my own practice part time. In 2003, I left my former employers to devote my full attention to my own practice and started my current group, City Footcare, PC.
‘Fast forward’ ten years to 2013 and I have developed and grown a thriving, successful group practice with four associate doctors under my supervision and guidance. I would not have been so successful without the support of you, my patients. In light of this success, I have chosen to change the focus of my practice going forward from general podiatry mixed with podiatric surgery, to predominantly podiatric surgery.
Focus on Podiatric Surgery:
It has always been my passion and goal to focus primarily on podiatric surgery. It takes many years to build a reputation as a great surgeon. I feel comfortable saying that I have already achieved this reputation at this point in my career. Right now, I am excited that this is the opportune time to act upon this success. Going forward I will be focusing my practice on podiatric surgery.
Practice Focus
I Will Continue to Accept New Patients for all Podiatric Problems:
I will not completely stop doing, general, non-surgical podiatry related care. I have formulated a way to spend a majority of my time performing surgery, including the preoperative and postoperative care related to surgery, while also practicing general podiatry some of the time.
I have assembled a team of excellent podiatrists in my City Footcare Group. I have hand-picked talented physicians who I have had the opportunity to work with for many years, and even train during their residencies. They have all spent time working with me in my office and observing my unique way of practicing podiatric medicine which has made my practice so successful.
Our physician group will work as a team to share in the care of our patients. I will help to oversee the care of patients who visit our practice. I will continue to see new patients a few days per week. During the initial visit, I will perform a detailed new patient visit including the patient’s history and physical examination. I will perform, order, and interpret the appropriate diagnostic tests. I will derive the diagnosis and start with appropriate treatments on the initial visit when indicated. When the treatments required are surgical, I will continue the care of the patients including preoperative consultation, performing surgery and all postoperative care.
When the treatment indicated is not surgical, I will direct the patients to follow-up with my partner doctors who will continue the necessary care. I will maintain communication with my partner doctors and provide any necessary input going forward.
To all of my existing patients, I would like to thank you for my success. It is because of you that I am where I am today. I know, and appreciate, that many of you will want to continue to see me, but I assure you that you are under the care of qualified physicians with my partner doctors. I will still be around to say hello or to provide any necessary input into your care.
I ask that you please respect my decision to make this change as it has been my career, and lifelong dream, to have a surgically oriented practice.
Sincerely,
Emanuel Sergi, DPM
Best Priced Custom Orthotics in NYC
We offer the best priced custom orthotics in NYC.
Many insurance plans cover the cost of Custom Molded Orthotics, but many also do not.
At City Footcare we like to be fair to our patients.

We make real custom orthotics in NYC, not modified over the counter, off the shelf insoles.
Not only are our orthotics the lowest price, but we like to think they are the best orthotics out there.
Dr. Sergi and associate doctors are experts in biomechanics of the foot. Biomechanics is the study of how the foot functions in gait, running and any weight bearing activity.
Call today to schedule a consultation and see for yourself how the lowest cost custom orthotics in Manhattan are also the best custom orthotics you can get.
(Click picture to enlarge)
Part II: British Hammertoes are “Wonky Toes”! Before and After Pictures of Hammertoe Surgery
British Patient with “Wonky Toes”
About 11 months ago I posted a blog post about my British Patient with “Wonky Toes”. I’ve had numerous requests to post the after surgery pictures of her hammertoe surgery and I finally have some time to do it.
Below is the original article in Blue. Scroll down to the new black text to see the additional information including after pictures.
ORIGINAL TEXT BELOW IN BLUE: Link: British Hammertoes are Wonky Toes.
A few weeks ago a lovely young woman came in to my office. She sat down with me in my exam room and proceeded to tell me in a wonderful British accent that her complaint was “Wonky toes”.
I guessed that she meant hammertoes but I wanted to clarify this before proceeding. I had never heard the term Wonky with or without toes after it. I asked her to clarify what she meant by wonky toes and she said, “you know like wonky teeth, crooked toes, crooked teeth.”
We had a good laugh and I had learned a new term. I asked her if I could blog about her and she agreed (obviously, as you *are* reading this).
My guess is that this post will be at the top of the search engines for wonky toes as I bet no one else is writing about wonky toes (at least in the US).
Fixing “Wonky Toes” – Wonky-Hammertoe Surgery.
My lovely patient had surgery yesterday for the diagnosis of hammertoe syndrome to correct two hammertoes. British translation: (read aloud in your best British accent) “This patient had surgery yesterday to correct two wonky toes in order to resolve her wonky toe syndrome.”
Pictures of her wonky toes are below. I’ll get the before and after hammertoe surgery pictures posted in a few months.
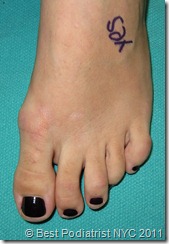 This picture (click to enlarge) shows the hammertoes of the fourth and fifth toes. The fourth toe is contracted down and under the third toe. The fifth toe is also contracted and rotated.
This picture (click to enlarge) shows the hammertoes of the fourth and fifth toes. The fourth toe is contracted down and under the third toe. The fifth toe is also contracted and rotated.
This is a picture of the same foot (click to enlarge) taken from another angle. You can see the third toe is elevated off the ground from the fourth toe residing underneath it. You can also see the fifth toenail is rotated forty five degrees relative to the ground.
I will be posting postoperative hammertoe surgery pictures soon…
I love when people post comments so please do not be shy. I will also personally answer all questions presented.
Thanks for reading, Lawrence.
Part II British Hammertoes are Wonky Toes 08/02/2012
This patient was very happy and satisfied with her hammertoe surgery. She said that the recovery was amazingly pain free. I’ve been treating her postoperatively for almost a year now. Her most recent photographs are from March 7th, 2012. This is 6 months postoperatively.
The recovery time for hammertoe surgery in order for the toes to be completely healed and the scar tissue to go down completely is usually around 9-12 months.
Before and after pictures of hammertoe surgery:
Below are pictures: 1) Before surgery. 2) Three days after surgery. 3) Two months after surgery. 4) Six months after surgery. (click any picture to enlarge)
This patient is scheduled to come back in September. I will post those pictures after her next visit.
Thanks for reading. Dr. Sergi.
When to have bunion surgery when you are not in pain.
My usual readers will know that I do not advocate bunion surgery for cosmetic reasons. My postings usually talk about bunion surgery to relieve pain. Both kinds of pain, shoe pressure and joint pain. (That reminds me of a classic scene from the movie Blues Brothers when the bartender says, “we have both kinds of music, country and western!)
I had a patient come in this week that I scheduled for bunion surgery that was not having pain. However, she was not scheduled for cosmetic reasons alone. She had severe bunions. She complained of not fitting into some shoes but she was okay with wearing less stylish shoes that did not hurt her bunions.
So, why would I schedule surgery on her if she had no pain and she did not complain of not fitting into shoes that she wanted to wear?
 On x-ray, she had signs of osteoarthritis in her great toe joints. Arthritis from bunions means that the cartilage in the great toe joint gets worn away. Often there is pain associated with it but sometimes there is not. (Click any picture to enlarge.)
On x-ray, she had signs of osteoarthritis in her great toe joints. Arthritis from bunions means that the cartilage in the great toe joint gets worn away. Often there is pain associated with it but sometimes there is not. (Click any picture to enlarge.)
Cartilage is the very smooth tissue on the ends of bones inside of the joints. Cartilage allows bones to glide with very little friction against each other in the joints.
On x-ray cartilage does not show up. It looks like clear space between the bones. When there is arthritis, the cartilage gets worn away and the bones appear closer together. When the cartilage is gone there is no space between the bones and they look like they are touching each other in the joints on x-ray.

 Clinically, when the cartilage is gone, one feels a grinding of the bones or what we call ‘crepitus’ in medical terms. By the time one has crepitus there is almost always pain associated with movement.
Clinically, when the cartilage is gone, one feels a grinding of the bones or what we call ‘crepitus’ in medical terms. By the time one has crepitus there is almost always pain associated with movement.
The reason bunions result in arthritis with wearing away of cartilage, is the joint is not functioning correctly. The bones intersect at an angle to each other and that results in uneven forces on the cartilage, causing erosion over time.
Let’s go back to my surgery patient who has no pain… She had signs of arthritis on her x-ray. The space between the bones was decreased. We call this joint space narrowing.
I advised her that she should have surgery because once the cartilage is gone, there is no way to get it back. Once this happens, patients require bigger surgical procedures and have a worse prognosis to be pain free after surgery.
There are basically two types of cartilage one can have in their (toe) joints: Hyaline cartilage and fibrous cartilage. Hyaline cartilage is the good kind that you are born with in your joints, and the kind I referred to above that gets worn away when one has arthritis. The second kind, fibrous cartilage, is not really cartilage in my opinion. It is more scar tissue inside the joints. When we (doctors) say we will do surgery to increase the cartilage, this is the kind we are referring to. We drill holes in the hard bone inside the joint in order to create the growth of fibrous cartilage as scar tissue from the drill holes in the bone.
Fibrous cartilage does not function as well as hyaline cartilage, but it at least forms a spacer between the bones that is softer than the bones rubbing on one another.
So, to answer my question above, I recommend bunion surgery to patients that have no pain when there is progressive cartilage erosion, with arthritis forming in the great toe joint.
The best hammertoe surgeon! (Including before and after pictures of hammertoe surgery)
This week I did a rather large hammertoe surgery. Additionally, I did another large hammertoe surgery on the same patient just six weeks prior on his other foot.
What do I consider a large hammertoe surgery versus a regular hammertoe surgery? This patient had some of the most severe hammertoes that I have ever operated on.
All eight of his toes, other than the great toes, were severely contracted. They were virtually dislocated at the metatarsal joint at 90 degree angles to the foot. The toe joints were dislocated in the opposite direction at 90 degrees and the second toe joints were in the opposite direction to that!
At this point, the below picture will do a better job describing what his foot looked like than my words. See pre-operative photos below of the left and right. (Click any pictures to enlarge and open in new window.)
Preop Left Foot Hammertoes.
Best Hammertoe Surgeon in NYC
Preop Right Foot Hammertoes.
Before I tell you more about the surgery and show you before and after pictures of this hammertoe surgery, let me tell you one amazing thing. The day of the second surgery, six weeks to the day after the first surgery, my patient informed me that he was playing basketball and comfortable the very day before.
Of course, I had told him it would be 12 weeks before he could play so he was not really listening to me, but I was happy he was doing so well after his surgery to recover so quickly.
This surgery was a big one as far as hammertoe surgery goes and he needed it on both feet. It was big because he required release and lengthening of 8 metatarsal phalangeal joints, 8 toe joints, 6 screws and 2 pins.
Let’s start at the beginning. If you want to skip ahead, scroll down and check out the before and after pictures of hammertoe surgery at the end.
This patient came to me with a complaint of pain in both feet at the toes due to the contracted joints. He had pain with any activity and just walking. He had trouble fitting shoes. He also didn’t like how they looked, and was embarrassed.
On physical exam he had rigidly contracted toes and dislocated joints. X-rays confirmed severe hammertoes and joint dislocations.
I told him all about the surgery to correct hammertoes and the postoperative course.
In surgery, I first opened up the to the toe joints and cut with a saw across the toe bones to shorten the toe and reduce the contracture of the toe joints. I then removed the cartilage of the adjacent bones in order to allow the two bones to fuse together when they heal and form one bone. This is necessary to achieve a very stable straight toe so that hammertoes will not come back again in the future after surgery.
People are always concerned when I talk about fusing bones and joints together as to what the future function will be. I describe it like this: The joints at the ball of the foot still function up and down. These are the important motions when walking, running and performing all activity.
The toe joints do not need to move. The toes are against the floor when you’re walking and running, etc. such that they do not bend anyway. The tendons still function to hold he toe against the ground but not bend into the ground. So, fusing the toe joints to never move again does not affect most activities going forward. It would be difficult to grasp with the toes like picking something up, but that’s not a usual activity for most of us.
Going back to the hammertoe surgery procedure, after I cut the bone and remove the cartilage in order to get the bones to fuse together, I then need to put in hardware to hold the bones in the proper place and position. There are multiple choices of hardware.
The old way to fixate hammertoes in surgery was to use pins called k-wires. While I occasionally do use these, they are not my first choice usually. K-wires hold the bones together in only one plane from angulating. The bones can still move from proximal to distal (close to far) on the pin which we refer to with an analogy of ‘food on a shishkabob’. It can move along the metal pin. It can also rotate on the pin.
New advancements in surgical fixation use metallic implants that are inserted into the bones to more rigidly hold them in place. These implants usually screw into one bone and are force fitted into the adjacent bone with barb-like structures. This prevents the bones from moving and rotating. I often use these but they are very expensive and do not hold as well as screws do.
Often, my fixation of choice are screws. Screws are unique in that they cause compression of the two bones to be fused together in order to hold them tightly together. This also stops angulation, and all other motion. I have found the greatest success rate of achieving fusion using screws compared to any other fixation.
So, by this time in the surgery, I’ve prepared the bones to fuse and then need to insert the screws. The special screws are called cannulated screws. The have a ‘cannula’, or hole down the center. This allows me to insert a temporary metal wire into the bones to hold them straight and to make sure I like the position before permanently fixing them.
Once I put the pins in and confirm I like the positioning with real-time x-rays, the screw slides onto the wire with the hole down the center. I screw the bones together and then remove the temporary wire leaving just the screw holding the bones together. You can see the screws on x-ray in the post-operative photos below.
Depending on the size of the bones I use different diameters and lengths of screws. Believe it or not, it is hard to find screws that are long enough for fusing toe bones. The problem in the past was that companies made shorter screws of the thinner diameters that did not allow for fusion of toes. The reason for this is that when fusing larger bones, we use thicker screws. There was no need for long thin screws. Fortunately, I was able to work with one of the screw companies in order to design special screws for the purpose of fusing hammertoes. This company makes screws that are longer than any other company. (Thanks Perry). If any doctors reading this want the name of the screw company, feel free to email me and I’ll let you know how to get these screws.
On the little toes, fifth digits, the bones are too small to safely insert screws without risk of fracturing the toes usually. For this reason, I usually do not use screws in the small bones but opt for k-wire fixation. I also do not fuse these bones but rather just take out part of the joint to shorten and straighten the toe. On some smaller patients this applies to the other toes too, not just the fifth toe.
Once the screws and pins are in and the toes are straight, I next address the base of the toe joint that is dislocated. I make another incision further back to access the next joint back. This is called the metatarsal phalangeal joint.
I lengthen the tendon that moves the toe up called the extensor digitorum longus tendon. This is an important step as this tendon has become permanently shortened over time, and that holds the toe upwards. I use a procedure called a Z-lengthening because the incision through the tendon is shaped like the letter Z. This allows the tendon to still function in a longer position after the toe is brought down. Next I go deeper to the joint capsule and perform a lengthening and release to bring the toe down from it’s upwardly contracted position.
At this time the toe is straight and the contractures are lengthened. The toe is shorter and in a perfect position. This is a really rewarding surgery for me. I take a severely deformed toe and turn it into a better looking and better functioning toe.
It took me just over two hours to do each foot, 4 toes including lots of plastic surgery maneuvers of the skin.
Most doctors would stop with straight toes but I have additional training in plastic surgery skin plasty procedures that I have written about on my blog before.
Imagine what happens when you shorten the bones drastically of these hammertoes. There is lots and lots of redundant skin and soft tissues left over. A big part of this surgery is obtaining a nice cosmetic outcome, as well as reducing pain and improving shoe fit.
In order to obtain a cosmetic foot surgery outcome, I spend a great deal of time working on the soft tissues, skin and suturing technique. First I shorten all the tendons and joint capsules that are redundant after the bones are shortened and suture them.
Next, I address the skin, in order to shorten the redundant excess. This involves a series of skin plasty procedures. I perform diamond shaped incisions to remove excess skin. I then perform additional smaller diamond shaped incisions at 90 degree angels to each other until the excess skin is gone and the toe is round again.
Even with all this plastic surgery type procedures, occasionally patients end up with small areas of excess skin postoperatively after the scar tissue forms. For this reason, I always inform patients that I can perform additional surgery nine to twelve months later, or more, to remove the excess skin in an additional surgery.
Ok, so to summarize: I’ve removed and shortened the bones. I’ve straightened the toes. I’ve permanently fused the bones with screws holding them together. I’ve reduced the soft tissue contractures at the further back joints. I’ve shorted the tendons and joint capsules. I’ve done plastic surgery skin plasty procedures for a cosmetic outcome and I’ve sutured everything with cosmetic surgery techniques.
You can see the drastic reduction of the hammertoes in the before and after photos. I always call my patients the next day after surgery. After both of these surgeries, I had expected this patient to have some post procedure pain, but was very surprised both times when he told me he had virtually no pain and took only one or two Vicodin.
As usual, thanks for reading and please submit comments and questions. Although I’m behind in answering them, I’ll eventually get to them all.
Before and after pictures of hammertoe surgery are below:
Left Foot:
 |  |  |
| Pre-op hammertoes surgery | Immediately post op hammertoes while still in surgery. | Two and a half weeks after hammertoe surgery. |
 |  |  |
| 7 Weeks after Hammertoe Surgery | 7 Weeks after Hammertoe Surgery | 7 Weeks after Hammertoe Surgery |
Right Foot:
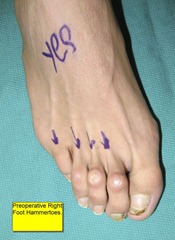 |  |
| Pre-op Hammertoe surgery | Immediately post op hammertoes while still in surgery. |
Side-by-side before and after hammertoe surgery:
 |
| Left Foot Top View |
 |
| Medial Side View |
 |
| Lateral Side View |
The best bunion surgeon and why!
Bunion Surgery
I strongly believe that bunion surgery is an art that necessitates the surgeon to adapt to the subject (the foot).
Our orthopedic text books clearly define all of our named surgical procedures and outline exactly how to perform them from the first incision down to bone and back to the skin closure.
Almost every foot surgeon that I’ve encountered from when I was a medical student, through surgical residency and now, as an attending physician, does surgery ‘by the book’. Most fail to adapt to the differences between patients and their deformities. Many fail to keep up with the new literature that describes the every changing medical landscape.
Medical journals describe new innovations, new medical devices, and doctors that report on how their patients do after new procedures. For decades this is how doctors have communicated their innovations. So, enough about other doctors, let me tell you about myself and my innovation. Interestingly, I believe this media, ‘blogging’ is the doctors’ communication of the future, better than medical journals.
In order to share, I will present a case study of a bunion surgery I did where I adapted to the patients foot, in this case, extra soft tissue after bunion removal.
What makes this bunion surgery innovative is how I adapted the incision to address the fact that after I moved and removed the bone, there was a large amount of redundant skin and deeper soft tissue left over. Nowhere in the podiatric literature is this problem addressed. In my training, I remember countless doctors saying that the extra skin will ‘resorb’ or go away on its own. I always thought to myself, how is that possible? How can extra skin and soft tissue just disappear into thin air? That defies the law of physics…
When I would see the postoperative results, I was not satisfied with that extra soft tissue left over after surgery. Sure, the pain from the bunion would go away and the patient could fit into shoes much better, but there was still that unsightly extra skin and soft tissue left over. I kept thinking, how can I solve this problem? Luckily, I was fortunate to have trained with plastic surgeons in my residency.
I learned valuable skills while working with them on face lifts, tummy tucks, and cosmetic breast surgery, that I have applied to my foot surgery. We like to call it ’tissue handling’ skills. The soft tissues of the foot are just like any other soft tissues of the body when it comes to surgery and suturing.
Here’s an example of the application of plastic surgery in foot surgery. A lovely young woman came to me with a complaint of an unsightly and painful bunion. She had progressively gotten more pain in her bunion over the years. At first, the pain was just with increased activity and spinning. Then, the pain would come with yoga and eventually, just walking.
When I examined her I found she had a pretty large bunion. We had an extensive discussion on ‘what is a bunion, what causes a bunion, and bunion surgery’. (For more info on bunions click the following link to a previous article I wrote: BUNION SURGERY INCLUDING BEFORE AND AFTER PICTURES
I described the procedure in detail to her and scheduled her bunion surgery procedure.
During bunion the surgery I cut and moved the metatarsal bone in order to remove the bunion.
After I moved the bone, there was lots of extra soft tissue remaining on the side of the foot from years of the bones protruding. Most doctors at this point would have stitched her up and left this extra soft tissue.
Honestly, most of these patients would be happy that their bunion was gone and the pain was gone and would have just lived with the extra soft tissue and just bought shoes that were larger to accommodate for this skin and soft tissue.
Unless they read this blog, they would not have known that they could have had an even better result if the surgeon simply knew how to perform two small procedures called a capsular debridement and a skin plasty.
Below are before and after pictures of this cosmetic bunion surgery. First is the preoperative picture. You can clearly see a large bunion. The first metatarsal bone sticks out the inside of the foot. The big toe angles toward the second and other toes. It looks unsightly and painful. (Click any picture to enlarge) (Sorry to call your foot unsightly C**** if you are reading this).
In the below foot x-ray of her bunion, you can see the first metatarsal bone is angulated to the side and the big toe leans toward the second and the other toes. Only part of the joint even touches the two bones together.

The only good thing here is that there is little to no arthritis in the joint. This patient came in early enough to avoid permanent painful foot arthritis from bunions.
Below is an intra-op picture of how I made this incision. First I made a traditional straight incision. Note also, that I make the incision on the side of the foot, not on top. I have described this incision on the side in a previous blog post on COMMON MISCONCEPTIONS OF FOOT SURGERY (click). There is no reason to put the incision on top where the scar is perfectly visible. I use this incision to access the bone and do the bunion surgery. After I have moved the bone and finished correcting the bunion, I then decide if I need to address any extra soft tissue. In this case I had extra capsule and extra skin. You can see where I then drew the diamond at the end of the incision. This is the skin I plan on removing in order to advance the reaming skin distally (further out) to reduce the ‘extra’ skin.
The first thing I do is remove any extra joint capsule by pulling the two edges together and cutting off any tissue that overlaps each other. This part is pretty easy. Next I close the deep tissue capsule with sutures. Next, I address the skin, which is a bit more complex as it is visible from the outside where the capsule is not.
In the picture you can see how I make an incision at an angle to the first incision at the end of the first incision. By making the two incisions at equal angles I can be sure the two ends will be the same length later when I close it.
I first make the distal incision first. I then pull the skin out towards the toe in order to determine how much extra skin needs to be removed. By pulling the skin out, I can determine how much to cut out by how much overlaps. This is the most important part, to remove the redundancy but not take too much skin. 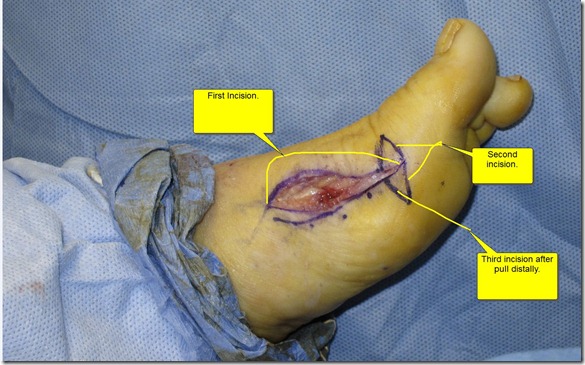
At this time, I then cut the skin to line up with the other end of the incision. (Note to any doctors trying this use the skin marker at first to draw it. Eventually you’ll get comfortable enough to do it with out drawing it first.) Now I have to carefully close the incision. First I close the subcutaneous layer (soft tissue superficial fascia layer just below the skin). I again employ techniques that I have learned from plastic surgeons. My suturing technique involves a very fine absorbable suture that I put literally in the edge of the skin. Absorbable suture means the body gets rid of it and I do not need to remove it. I do, however, have to remove the two knots on each end of the suture.
I used to bury the knots inside but I found that the extra suture material at the knot caused a bump inside at the ends of the incision. I do the knots externally now.
While suturing, the skin is pulled out to be taught over where the bunion used to be. In the below picture after suturing, you can see how there is no extra skin where the large bump of bone used to be. You can also see that the previous angled incisions have pulled to the center to be at 90 degrees to the main incision. You can see the incision is shaped like a ‘T’ on its side.
The next picture, below, is at ten months after the bunion surgery has healed. There is still a small amount of induration, scar tissue, that will go away slowly. The induration still makes the foot look slightly swollen. You can see the scar where the ‘T’ shaped incision was.

Below are before and after pictures of her bunion surgery at ten months postop. On follow-up this patient reported that she was pain free with walking, yoga and spinning. She was very happy with the outcome both cosmetically and with relief from the pain. As always, it was a little sad for me to say good-bye after a year of seeing her and getting to know her, but she reminded me that she may be back for her other foot…
Thanks for reading. Please write comments. I will try hard to find time to write back. It may take a while, but I’ll do it.
If there are any doctors out there that emulate my incision ideas above, please let me know how it worked out!
Lawrence
Skiing (foot) tips from a podiatrist
I recently went skiing in Whistler-Blackcomb Mountain, British Columbia, Canada. Ironically, I suffered from toe pain on my first day on the mountain.
This ironic injury gave me the idea to write a blog on how to protect your feet when skiing. I also figured it would be nice to share a little about my personal life with my blog readers by posting pictures and video of skiing at Whistler, the best skiing I’ve ever done. (Pictures and video are at the bottom below.)
We spent 1.5 days in Vancouver prior to going skiing. As almost expected, it rained a lot of the time there. We explored the city on foot and by car and then drove Route 99 the “Sea to Sky Highway” up to Whistler.
This scenic drive allows you to see the fjords where the mountains meet the water. 
We stayed right at the base of the Mountain at the beautiful Westin Hotel. We rented skis and boots at their ski shop which brings me to my first podiatric skiing tip:
Boot rental… The technician measured my feet and brought me a boot. The boot fit well except for the fact that I thought my left big toe was hitting the front end of the boot inside. The technician instructed me to stand up and lean forward and if my toe did not hit the boot at that time, then the boot was the proper fit.
When I leaned forward standing, the toe no longer felt like it was hitting the front of the boot so I took his advice and took the pair of boots he recommended for skiing the next day…
That night I decided to cut my toenails short so that the nail did not stick out any further than the skin of the tip of the toe. This is tip number one, cut your nails prior to skiing. I have seen many people with toenail injuries from tight footwear when participating in sports and recreation.
Often, tight footwear puts pressure on the nail and pushes it slightly up and back with every step or other movement like skiing. Often the person feels nothing as the nail slowly separates from the skin below it, called the nail bed. Repetitive forces cause the nail to separate and blood to accumulate under the nail. Most times with no pain, the nail turns black as the blood fills the area.
Additionally, often there is no discoloration or blood under the nail, but rather a colorless fluid fills the area under the nail in the same manner as a blister forms in the skin. Whether it’s blood or a blister, the results are the same. The nail separates from the skin and eventually falls off.
We often estimate that if 75% or more of the nail separates, then the person will eventually lose the entire nail. Most often this occurs over 1-3 months after the injury.
In my case the nail did not separate but it was sore after my first day of skiing. I believe by cutting my nails the night before, I escaped this more severe injury. At the end of the first day, I went back to the rental place and exchanged my boots for the next larger size. The boot no longer pressed on the big toe but the boot was a little bit too large and my heel elevated slightly when leaning forward. To alleviate that, I just wore a second pair of socks and then the boots fit perfectly for the next three days of skiing. I guess that’s tip number one point five; when the ski boot is a bit too large, wear an extra pair of socks instead of getting a smaller boot.
The next tip addresses arch pain. Often people with arches that collapse get pain, soreness or fatigue of the arches when skiing. Ski boots, like most other shoes and boots, do not have great arch support. Spending 4-8 hours skiing in rigid boots is similar to standing in one place for hours at a time as the foot is locked and immobilized in the hard boot.
In order to alleviate this soreness or pain, I recommend using insoles in the boot which is tip number two.
Different people will respond differently to the type of insoles one uses.The first are soft insoles. These soft insoles are the ones you can buy in the pharmacy which are just cushions and not arch supports. These offer the least arch control and the most cushion of the ones I recommend.
The next type sacrifice cushioning slightly and are over the counter, non-custom arch supports that are slightly more rigid than just the cushions. These offer some control of the arch and some cushioning.
There are also more rigid over the counter insoles that one can buy that offer even less cushion and more arch control. Because these are generic and not custom, they will only fit into the arch of some people that have arches that are not too high nor too low. Many people will not feel comfortable with these and feel like there is a hard ball under the foot.
The final type of insole are custom molded orthotics that I make in my office by taking a mold of the foot and sending it to my laboratory. With these I can make them as hard or as soft as I determine is necessary based on my physical examination of the patient and professional opinion. These also are the exact shape of the persons arch.
The next tip is kind of common sense but you’d be surprised how many patients I’ve seen that lack enough of it to follow this simple tip. If you’re having pain, you’re doing harm. This applies to other parts of the body too when skiing. Don’t ‘work through pain’. Address that foot pain or knee pain by seeing a doctor before you cause more significant harm and become harder to treat.
The last tip is to pay attention to frostbite. While I admit that I don’t see too many frostbite patients in New York City, it does often happen to the feet in colder climates when skiing. Frostbite can cause permanent problems and even amputation. If your ‘feet are freezing’ they might actually be freezing. This is especially dangerous for people with peripheral vascular disease and worst for people with Reynaud’s disease.
Okay, enough of the podiatry skiing tips for now, let’s talk about the incredible skiing at Whistler-Blackcomb. We got lucky with a really nice week of snowfall just prior to our arrival. We enjoyed skiing amazing powder conditions and even had lots of fresh snowfall while we were there.
Below are pictures and videos of our trip. (click to enlarge)
Videos: (Tip: double click the videos to watch in YouTube, faster download)
I hope you enjoyed sharing my ski vacation and reading about foot health while skiing.
Please feel free to leave any comments or questions. Dr. Sergi
What is a Neuroma? How do you treat Neuromas? and, Alternatives to Neuroma Surgery when conservative treatment fails. Radiofrequency Ablation for Neuroma.
A neuroma is an inflamed, enlarged nerve. Many problems that end in -oma are tumors but this one is not. Neuromas can occur at any nerve in the body but are very common in the foot, which are the ones I will discuss.
Neuromas are most often found in the common metatarsal nerves of the foot which are the nerves just behind the toes. The job of these nerves is to allow you to feel one side of each of the adjacent toe. For example, the metatarsal nerve between the third and fourth toes allows you to feel the sensation on one side of the third toe and the adjacent side of the fourth toe. These nerves do not connect to any muscles, they are just for sensation.
A neuroma forms when the nerve is pressed upon by the adjacent structures. The four surrounding sides of the nerve are made up of: The two metatarsal bones next to the nerve to the left and right. The top border is a ligament connecting and holding together the two adjacent metatarsals called the ‘deep transverse intermetatarsal ligament’. The bottom structure is the skin and the ground below it.
This space defined above is a small place for the nerve to pass along with tendons. Pressure when walking hurts this inflamed nerve. Most people describe the pain as intermittent and ranges from mild to severe. I often hear it described as pain, numbness and tingling that shoots into two toes. Many people describe an uncomfortable fullness between their toes.
People can have neuroma pain in multiple interspaces and in both feet or just one spot. The most common place is between the third and fourth toes and the second most common place is between the second and third toes. Neuromas are very rare in the the first and fourth interespace.
Neuromas between the third and fourth toes are called “Morton’s Neuromas”. Dr. Morton named this neuroma after himself because they are so predominantly found between the third and fourth toes. The reason for this is that the third interspace nerve is naturally larger than the others and is more likely to become inflamed and painful.
People with arches that collapse (pronate) or flat feet are more likely to get neuromas. When the foot pronates and the arch collapses, the foot moves slightly toward the side, toward the little toe. This puts horizontal forces on the metatarsal bones pushing them together.
Women who wear heels are more likely to get neuromas because the high heels tilt the foot forward putting more direct pressure up on the nerve. People who wear tight shoes in the forefoot also get neuromas as the shoes push the metatarsal bones together.
So now that we have described what neuromas are, why we get neuromas and neuroma symptoms, let’s discuss treatment for neuromas.
The first line of treatment is anti-inflammatory measures in order to decrease pain and make the enlarged, inflamed nerve smaller. This first line of treatment includes prescription and over the counter anti-inflammatory pills, icing, and corticosteroid (‘cortisone-like’) injections.
Often, I will give an injection on the first visit. Injections work very well and very quickly to get rid of neuromas. Unfortunately, there are side effects of steroid injections. Usually one injection will not have adverse effects but I have seen it happen. These adverse side effects of steroid injection include local atrophy (weakening) of soft tissues such as ligaments and tendons. Weakening can lead to injury and rupture of these structures. I do not like to give more than three steroid injections in the same spot within twelve months. Other side effects of steroid injections include fat atrophy where a small indent forms between the bones where the injection takes place because the natural fat below the skin atrophies. This can be permanent or temporary. An additional side effect of steroid injections is loss of pigment in the skin. This can happen just in the area of the injection or it can travel along the lymphatic and vein structures causing a streaking effect. This usually only effects people with darker skin and more pigment.
Again, these are side effects that rarely happen but can occur. I discuss these with patients prior to injecting. Due to these potential problems, I try not to perform injections on the first visit and try alternative treatments first. With that said, I do perform these injections regularly on the first visit. I do them when the patients are in severe pain and want quick relief from the pain they are suffering from as the injection is the quickest and one of the most effective ways of getting rid of painful neuromas.
In my experience a majority of the people that are treated with icing and oral anti-inflammatories return for an injection on the subsequent visits.
The next line of treatment involves a longer approach to eliminating the forces that cause neuroma. This is done with custom or over-the-counter orthotics. Sometimes just a pad alone in the shoe can reduce the pressure by pushing the metatarsal bones apart and off the nerve, but a custom orthotic does this as well as addresses the collapsing arch.
When all the above treatments fail, my next treatment is physical therapy. Physical therapist perform anti-inflammatory ‘modalities’ to try to reduce the inflammation of the nerve.
When all the above and PT fail to treat neuromas then we discuss a little more invasive procedures. Surgery for neuromas is the last resort. There are some newer procedures that we call minimally invasive procedures for neuromas. Please do not confuse this with minimally invasive bone surgery of the foot which I discussed in detail of the perils of it, in my previous blog.
There are a few minimally invasive procedures for neuromas:
My favorite procedure is called ‘Radiofrequency Ablation for Neuromas’. I have been doing this amazing procedure for a few years and I have close to one hundred percent success with it. This involves inserting a radiofrequency probe into the foot right at the inflamed nerve. Once it is in the perfect spot, I heat up the tip of the probe to ninety degrees Celsius, just below the boiling point of water. I repeat this process at three areas of the neuroma, all through one entry point through the skin. This pin point spot of heat denatures the proteins off the nerve and stops the transmission of the pain fibers.
Occasionally, there is a result of numbness or decreased sensation in the two adjacent toes, but that is rare and when it does happen, people have always told me that a tiny amount of numbness is better than pain.
Radiofrequency ablation for neuromas is a relatively painless procedure that requires just one or two injections that hurt less than a typical steroid neuroma injection.
Recovery after radiofrequency ablation for neuroma is pretty easy as well. Healing time is very short as there are no incisions to heal. Patients do not need to worry about keeping a foot dry for this reason, and can get it wet and shower immediately after the procedure. Additionally, I only recommend patients stay of their foot the night of the procedure and rest only if there is discomfort for one to two days after. Most people report mild soreness or throbbing for one to two days after. Many people have no discomfort at all afterwards.
After radiofrequency procedures I tell patients that they may see immediate relief of the neuroma pain within one to five days. I also inform them that some people require up to three months for the procedure to work. I do not call it a failure until three months have passed and the pain is still the same as prior to the procedure. When people report no relief at two months, I will repeat the radiofrequency procedure at that point. If they have some relief I tell them to wait a full three months. If they still have some or all of the pain at three months, I repeat it then. I have done one, two and three procedures on people so far and have almost a perfect record.
Other minimally invasive procedures for neuroma include a series of seven to ten sclerosing alcohol injections, cryosurgery for neuromas, and a nerve decompression procedure often called a ‘kobygard’ procedure. I’ve done them all in the past and prefer the radiofrequency over them all. The alcohol injections did not work very well with only a handful of patients having any relief. The cryosurgery procedure worked okay but people had significantly more post procedure pain than radiofrequency and no where close to the success rate. Cryosurgery for neuromas is also done in the hospital or surgery center while radiofrequency is done in my office. Lastly, the kobygard procedure had a better success rate than the cryo or alcohol but not as good as the radiofrequency. Kobygard decompression is also done in the hospital or surgery center and is more invasive requiring a small incision between the toes and suturing. This means you need to keep the foot dry for twelve days after surgery. Patients also experience much more post procedure pain than the radiofrequency as well.
The last option is surgical removal of the neuroma. This is a great procedure when it its needed but as you can tell since I’ve started doing the radiofrequency procedure I have not had to do many open surgeries. This surgery involves an incision on the top of the foot and dissection down to the nerve below the ligament. I then remove the enlarged area of nerve and close up the foot.
When I do these surgeries, the nerve is very enlarged. To give you an analogy of what it looks like, a normal nerve looks like a piece of spaghetti’s thickness. A neuroma looks like the size of a jelly bean attached to the nerve. Depending on the severity it ranges from a Jelly Belly small candy to a traditional large jelly bean in size.
Okay, that’s about it for neuromas today. To summarize, neuromas are enlarged nerves caused by mechanical irritation. They can be very painful and annoying. We’ve discussed conservative, non surgical treatment as well as minimally invasive treatment and finally surgical treatment of neuromas.
As always, I hope this help and feel free to comment. I will do my best to reply in a timely manner.
Dr. Sergi
What is gout? and… Foot surgery for gout.
Last week I performed surgery on a patient for gout. Well, for a gouty tophus actually. Gout is a metabolic disease that requires pharmacological treatment and diet changes, not surgery.
Surgery is, however, indicated for the symptoms that go along with gout. First I will tell you a little about gout in layman’s terms, then I’ll discuss complications of gout in the foot and finally gout surgery.
What is gout?
Gout is a metabolic disorder in which there is too much uric acid in the blood. This can come from: taking in too much protein that is broken down into uric acid; the kidney not being able to process enough uric acid to excrete it in the urine; and thus uric acid builds up in the blood, or less commonly, the body producing too much uric acid.
Uric acid in the blood comes from the breakdown of purines from our diet. Purines are part of proteins and are more abundant in some foods than others. The biggest offenders are shellfish, organ & red meat and legumes (beans). Alcohol intake competes in the kidney and makes the kidney excrete less uric acid than normal.
Once we intake protein, it is converted to purines and pyrimidines and the purines are further broken down in uric acid and other byproducts. The uric acid is removed from the blood by the kidney. When not enough uric acid is removed, it builds up.
High uric acid alone does not cause symptoms, however, it can effect the kidney. Being a podiatrist, I’ll skip the systemic effects of gout and talk about the manifestations in the foot.
What is an acute gout attack?
An acute gout attack in the foot occurs when the uric acid comes out of the blood and into the joints, usually the great toe joint of the foot.
If you think real hard and try to remember back to high school chemistry, a liquid can only hold some amount of a solid dissolved in it. Once it reaches its saturation point, it cannot hold any more.
Another fact about solids dissolved in liquids is that a warmer liquid can hold more solid dissolved in it than the same liquid when it is cold. Picture dissolving sugar in hot coffee which goes pretty easy, versus trying to dissolve sugar in cold water.
Going back to gout and stop reminiscing about high school, uric acid is the solid and blood is the liquid. When the blood gets further away from our core and into the extremities, it gets cooler. The warmer blood that was holding all of that uric acid dissolved in it can no longer hold all of it. For unknown reasons, the uric acid then comes out of the blood and into the joints as a solid in the form of a solid crystal.
These uric acid crystals are called negative biorefringent crystals because of how they reflect light when looked at under a microscope, but that goes beyond the scope of this article.
When these uric acid crystals enter the joints the fun begins. The body mounts a major immune response as these crystals are not supposed to be in there and are looked at like a foreign body. This is what is called the acute gout attack.
Symptoms of an acute gout attack are usually severe pain in and around the joint. The joint appears angry. It gets red, hot and swollen. Any light touch or motion hurts. Many people tell me that the pain starts at night and just the pressure from the bed sheets hurts.
Often people present with symptoms that mimic an injury but cannot recall any trauma. Often gout is also confused with the red, hot swollen symptoms of infection but there is no open sore or injury where bacteria can get in.
Making the diagnosis of acute gout attack:
Most of the time I diagnose gout based on history and symptoms. Again, red, hot swollen, painful foot joints without history of trauma or infection. Most acute gout attacks occur in the great toe joint and other joints of the foot and ankle. The next most common joint affected is the knee, however, gout can occur in any joint in the body.
Most of the time when I suspect gout, I will do a blood test to measure the serum uric acid, however, this is not always a great test. Often the serum uric acid is normal even during an acute gout attack. When the uric acid blood test is normal you cannot exclude gout as your diagnosis, however, if the serum uric acid is high then you do have your diagnosis. Medically, we call this a false negative when the uric acid is normal but it really is gout. We also say that this blood test “can rule gout in but cannot rule out gout”.
The most accurate way to diagnose gout is to pull fluid out of the painful joint with a rather large needle. I rarely do this because it hurts a lot. Also, the great toe joint is a small joint with very little fluid and it is really hard to get any fluid out of it. When fluid is taken out of the joint, the pathologist looks under a microscope to see if there are uric acid crystals in it. Normally there are none so if he/she sees any, you definitely have gout.
Acute gout attack treatment:
The first line of treatment is anti-inflammatory medications. The old anti-inflammatory medicine used is Colchicine. Personally, I rarely use colchicine but it is still an acceptable treatment method used today. The reason I don’t use colchicine is because it causes side effects. Patients are told to continue the colchicine until either they vomit or have diarrhea, whichever comes first. Both not very pleasant sequelae.
Instead of colchicine, I use Indomethacin (aka Indocin). Indomethacin is in the same class of drugs as aspirin or Motrin but is stronger. For unknown reasons it works better on gout attacks than other anti-inflammatory drugs in the same class. Other anti-inflammatory drugs work well too, but I find Indomethacin to work the best. I prescribe Indomethacin 50mg, one by mouth three times a day for the first 4-5 days, then twice a day for up to 7-8 days. It is taken with food. I tell patients to stop it when the pain subsides or they reach 7-8 days and then follow up.
When people cannot tolerate Indomethacin because of stomach problems, I usually prescribe Celebrex. Celebrex is in a class of anti-inflammatory drugs called Cox-2 inhibiters. These drugs have less adverse effects on the stomach.
Another treatment is steroid injection into the joint. I do this when the symptoms are really severe. The steroid injection is a very strong anti-inflammatory, placed exactly where the inflammation is. It works almost immediately usually to resolve the pain. Unfortunately, it hurts going in. I have to stick a needle into an already painful, inflamed joint.
Oral steroids also work well but have more side effects than the Indomethacin. Icing the painful area will help as well. Resting the effected joint with decrease pain too.
Long term treatment involves oral medications to prevent the build up of uric acid in the blood. Again, as a podiatrist, I will skip this as it exceeds the scope of my blog post. One thing I will write about this is, do not take these uric acid lowering medicines while in the acute stages of gout as they often make the gouty attack worse.
Below are pictures of the gouty tophus that I took out. This is the result of many years of build up of uric acid in and around a joint.
Thanks for reading and I hope I’ve helped. The subject of gout is huge and I could have written many times as much as this already long post…
Below are two pre-operative pictures of gout (click any picture to enlarge):
Below are intra-op pictures of the gouty tophus coming out:
And finally below is a picture of the gout tophus once it was removed from the foot:
And, lastly, below is a picture from a different surgery. This is a picture of uric acid crystals, gouty tophus, I encountered when doing bunion surgery. I did not expect to see this as they patient never had a history of any gout attacks, however, apparently, he had chronic gout and did not know it.
Lawrence
Celebrity Podiatrist
 While it is exciting to be a ‘Celebrity Podiatrist’, we treat all of our patients like celebrities and with respect. We appreciate the trust they put in us.
Almost daily I get podiatry questions from this blog, from people all over the world. Many people book travel to NYC in order for me to treat them and operate on them. I often do surgery on people who spend three to four weeks here in NYC recovering.
In the past two decades of practice I have treated many ‘high profile’ patients including: actors and actresses, reporters, celebrities, scientists, inventors, diplomats, radio personalities, professional and amateur athletes, professional wrestlers, CEOs, other doctors, attorneys, authors and many other interesting people.
My current patients will agree that I get to know my patients. I pride myself on being knowledgeable about many subjects. I often talk about many personal matters with my patients during their podiatric visits. I really enjoy getting to know people and learning from them.
My friend and I always joke about how different out medical practices are. My friend is an emergency medicine doctor at a large level one trauma center in Brooklyn. A very different environment than my fancy Madison Avenue office. He fixes people, and sends them out on their way and usually never sees them again. I, on the other hand, enjoy getting to know my patients and often build a long lasting relationship with them. I really enjoy this part of my practice.
Thank you to all my current patients for making my practice successful, and I look forward to meeting the rest of you.
Emanuel Sergi
While it is exciting to be a ‘Celebrity Podiatrist’, we treat all of our patients like celebrities and with respect. We appreciate the trust they put in us.
Almost daily I get podiatry questions from this blog, from people all over the world. Many people book travel to NYC in order for me to treat them and operate on them. I often do surgery on people who spend three to four weeks here in NYC recovering.
In the past two decades of practice I have treated many ‘high profile’ patients including: actors and actresses, reporters, celebrities, scientists, inventors, diplomats, radio personalities, professional and amateur athletes, professional wrestlers, CEOs, other doctors, attorneys, authors and many other interesting people.
My current patients will agree that I get to know my patients. I pride myself on being knowledgeable about many subjects. I often talk about many personal matters with my patients during their podiatric visits. I really enjoy getting to know people and learning from them.
My friend and I always joke about how different out medical practices are. My friend is an emergency medicine doctor at a large level one trauma center in Brooklyn. A very different environment than my fancy Madison Avenue office. He fixes people, and sends them out on their way and usually never sees them again. I, on the other hand, enjoy getting to know my patients and often build a long lasting relationship with them. I really enjoy this part of my practice.
Thank you to all my current patients for making my practice successful, and I look forward to meeting the rest of you.
Emanuel SergiBritish Hammertoes are “Wonky Toes”!
A few weeks ago a lovely young woman came in to my office. She sat down with me in my exam room and proceeded to tell me in a wonderful British accent that her complaint was "Wonky toes".
I guessed that she meant hammertoes but I wanted to clarify this before proceeding. I had never heard the term Wonky with or without toes after it. I asked her to clarify what she meant by wonky toes and she said, "you know like wonky teeth, crooked toes, crooked teeth."
We had a good laugh and I had learned a new term. I asked her if I could blog about her and she agreed (obviously, as you *are* reading this).
My guess is that this post will be at the top of the search engines for wonky toes as I bet no one else is writing about wonky toes (at least in the US).
Fixing “Wonky Toes” – Wonky-Hammertoe Surgery.
My lovely patient had surgery yesterday for the diagnosis of hammertoe syndrome to correct two hammertoes. British translation: (read aloud in your best British accent) “This patient had surgery yesterday to correct two wonky toes in order to resolve her wonky toe syndrome.”
Pictures of her wonky toes are below. I’ll get the before and after hammertoe surgery pictures posted in a few months.
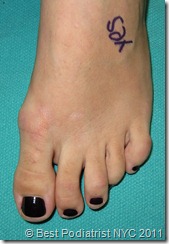 This picture (click to enlarge) shows the hammertoes of the fourth and fifth toes. The fourth toe is contracted down and under the third toe. The fifth toe is also contracted and rotated.
This picture (click to enlarge) shows the hammertoes of the fourth and fifth toes. The fourth toe is contracted down and under the third toe. The fifth toe is also contracted and rotated.
This is a picture of the same foot (click to enlarge) taken from another angle. You can see the third toe is elevated off the ground from the fourth toe residing underneath it. You can also see the fifth toenail is rotated forty five degrees relative to the ground.
I will be posting postoperative hammertoe surgery pictures soon…
I love when people post comments so please do not be shy. I will also personally answer all questions presented.
Thanks for reading, Lawrence.
Ethical laser nail fungus treatment (and topical treatment for nail separation)
This week I turned down three patients for laser nail fungus treatment. That’s right, I told three people NOT to pay me $600 each, $1800!
All three had separation of the nail form the nail bed soft tissue attachment. This causes the nail to look different in color in the area that it is separated.
This discoloration of the nail looks like nail fungus to the untrained eye. Very often, people come to my office with this separation of the nail from the nail bed, thinking it is fungus when it is not!
Laser will not fix this problem. Neither will topical medicines alone.
Treatment for separation of nails:
The only fix for this is to remove the part of the nail that is separated, all the way back to the area of good soft tissue attachment with cutting and grinding of the nail.
Once this removal is performed, then I advise patients to use topical medicine for the nails. I have formulated my own topical medicine for this purpose. This medicine also has an anti fungal medicine in it.
My product is called NailPure by Dr. Silverberg. The anti fungal ingredient is Tolnaftate. The multiple oil vehicle allows the Tolnaftate to penetrate the hard nail plate to reach the fungus.
In the case of nail plate separation, however, it’s not the anti fungal that is important. It is the multiple oil vehicle. It contains tea tree oil, manuka tree oil, jojoba oil, sunflower seed oil, and sweet almond oil (and vitamin E). This unique combination of essential oils penetrate, emulsify, soften and hydrate the nail and surrounding skin. Additionally, NailPure contains acetic acid that whitens the nail to make it appear more normal very quickly. Acetic acid is a natural acid that makes vinegar have its characteristic smell and taste.
By treating the skin and nail, NailPure allows the nail to grow in and reattach to the nail bed having normal color and looking healthy.
The best topical antifungal for nails also works on nail bed separation:
Wow, what a tangent! I was talking about doing the right thing for these three patients, and got excited about introducing my new topical nail fungus treatment. I spent one and a half years working with my chemist in Florida to perfect NailPure. I tried many different combinations of ingredients and vehicles until I came up with the proper formula. I tested it on dozens of my patients and waited patiently while their nails grew in healthier without fungus, whiter, thinner, and more clear. I then discovered how well it worked for nails that were separated from the nail bed. I used to use topical urea gel or cream for these patients but I discovered that NailPure worked so much better.
Honestly, when I started developing NailPure, I did not think to use if for nail separation, but when I discovered how well the oil vehicle worked on the nail and skin, it was obvious. I had stumbled upon a new, amazing treatment for a previously very difficult problem to solve.
Going back to my original topic, these three patients were very grateful that I saved them *$531 by not performing the laser for nail fungus, that would have been unsuccessful. *Note: $600 minus $69 for the NailPure.
Unfortunately, many doctors as not as honest, ethical and altruistic as I am. They would have performed the laser nail fungus treatment for the money. You see, studies have shown the laser nail fungus treatment to be 70-80% effective. These doctors hide behind that statistic and tell these people that is why the laser did not work.
Other doctors may be mistaken to make an improper diagnosis of nail fungus when in fact it is separation of the nail plate. In my opinion, this is why many nail fungus treatments fail. It was never fungus.
Choosing a provider for Laser Nail Fungus Treatment:
In summary, when choosing a provider to take care of your nail fungus, make sure you go to a doctor that you know and trust. Get a recommendation from a friend or another doctor (or come to NYC to my practice). Question your doctor about if it is really nail fungus or separation of the nail plate. When in doubt, your doctor will send a (painless) clipping to the lab for evaluation under the microscope. And lastly, be weary of doctors advertising for laser nail fungus treatments. A doctor spending money on advertising will be looking for return on investment and willing to perform lasers on everyone that comes through the door inquiring. Keep in mind too, that the lasers are very expense pieces of equipment and doctors will be looking to pay off their leases… However, with all at said, most doctors are still ethical. There are just a few that are not to look out for.
As always, feel free to send me email questions on this topic. Dr. Sergi
Hammertoe Surgery
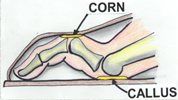 Many people seek the help of their doctor in hopes of fixing their hammertoes. It is common for podiatrists to receive patients who want to do something about their “ugly toes.” In truth, hammertoes can also be quite uncomfortable when they lead to such thing as painful corns, calluses, and swelling. The good news is that we will be able to perform toe surgery if necessary.
Many people seek the help of their doctor in hopes of fixing their hammertoes. It is common for podiatrists to receive patients who want to do something about their “ugly toes.” In truth, hammertoes can also be quite uncomfortable when they lead to such thing as painful corns, calluses, and swelling. The good news is that we will be able to perform toe surgery if necessary.
Depending on what stage the deformity is in, a hammertoe can be either flexible or rigid. When they become painful hammertoe surgery will be necessary to alleviate the problem.
Different Types of Hammertoe Surgery
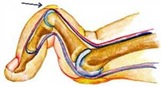 Surgeries to correct hammertoes do not require an overnight stay at a hospital. The procedure can be done during the day and then you can go home to recover. Essentially, you are given either just a local anesthetic or sedation so that you can sleep through the procedure. Such surgery only requires a small incision. The different types of hammertoe surgery are soft tissue correction, digital arthroplasty (removal of a small piece of bone), and digital arthrodesis (joint fusion).
Surgeries to correct hammertoes do not require an overnight stay at a hospital. The procedure can be done during the day and then you can go home to recover. Essentially, you are given either just a local anesthetic or sedation so that you can sleep through the procedure. Such surgery only requires a small incision. The different types of hammertoe surgery are soft tissue correction, digital arthroplasty (removal of a small piece of bone), and digital arthrodesis (joint fusion).
Soft tissue corrective surgery redirects the tendons and joint capsule of your toe which will correct the position.
A physician will have to implement a combination of procedures using techniques from the different types of toe surgeries mentioned. Digital arthroplasty involves correcting the soft tissue and removing a piece of bone in order to straighten the toe. Digital arthrodesis techniques involved fusing two bones together in order to straighten the toe. Often hammertoe surgery requires a mental wire or other implant to be inserted into the toe that will hold it into place while it heals. The end result will be a straightened toe.
How Long Does it Take to Recover from Hammertoe Surgery?
I do most of my surgeries on Friday. I instructed patient to remain off their feet all day Friday, Saturday and Sunday. People that have a desk job can usually return to work on the Monday following their Friday surgery. Most people wear a surgical shoe for 3-4 weeks.
Before surgery, make sure that you have a friend or family member who can bring you home after the procedure. It’s important that you take proper care of your feet in the weeks following the procedure in order to get the most out of your surgery. This will involve wearing proper footwear and following the instructions given.
Common misconceptions about foot surgery
While I was writing my last post on hammertoe surgery it occurred to me to write a post on common misconceptions of foot surgery.
(Don’t feel like reading a long post? Skip to the last paragraph for a quick summary.)
1) The first one was one that I mentioned in my last post: that extra skin left behind in surgery reabsorbs. This is preached by many foot surgeons but is entirely untrue. Skin left behind remains extra skin after the swelling and scar tissue go down. It is true in the short term that you may not notice it because the area is swollen and the skin is expanded but once the size of the area goes down you still have extra skin.
A small exception to this is when we do hammertoe surgery for corns, sometimes we have to leave part of the corn behind because the skin incision would be too large to close if we cut out the whole corn. After the hammertoe surgery, the pressure and rubbing on the shoe that caused the corn is gone. In this case, the thick hard skin that makes up the corn will go away after surgery. However, this assumes that the correct amount of skin was removed, including the corn. If extra skin remains at the incision, even though the hard part will go away, the extra skin will not go away.
2) The next misconception is also somewhat of a cosmetic one. Many foot surgeons say they put the incision for bunion surgery on the top of the foot because if they put it on the side where it is hidden more, it will rub on the shoe and cause discomfort. Last time I looked at a shoe it encountered the foot on four sides not just one. The real reason doctors put the incision on the top of the foot for bunion surgery is just because they were taught that way when they learned surgery. It also makes it slightly easier to do the surgery, so the surgeon can more easily access the side of the great toe joint closer to the second toe in order to release the soft tissue contracture there. This creates an unsightly scar when looking down on the foot. A much more cosmetic way to do it, is to put the incision on the side of the foot so when looking down you don’t see the scar. With some finesse, I can still easily access the other side of the joint and if I need even more access, I can make a tiny incision between the first and second toe that is barely noticeable.
3) The next misconception: minimally invasive bunion surgery (or other minimally invasive foot surgery) is superior to regular open surgery. The truth is quite the opposite! Minimally invasive surgery entails using a small drill to cut the bones through small stab incisions while visualizing the drills under real time x-rays (Fluoroscopy). This type of surgery is very imprecise as to how much bone is removed and where the cuts are made. I have seen many of these patients have complications due to taking out too much bone and shortening the metatarsal too much, or even not taking enough bone. In addition it is impossible to fixate the cut bone with screws in order to get the bone to heal in the proper place. Some of the doctors that do this type of surgery use ‘percutaneous pins’ in order to hold the bone. This means the pins go through the skin and into the bone. The pin remains sticking out of the skin for 4 to 6 weeks after surgery in order for the bone to heal. The downside to this is that you need to keep the foot dry the whole time the pin is sticking out. Also, the pin exit point creates an additional scar. Additionally, as long as the pin sticks out through the skin, a patient may get a “pin tract infection”. This is when the bacteria from outside the body goes down the pin and into the foot, and into the bone. When you get bacteria or infection in the bone you have a serious problem and need the bone removed, the use of IV antibiotics and usually requires hospitalization. When a screw is used it is completely inside the foot and a patient may get the foot wet after about one and a half to two weeks. Most doctors that perform minimally invasive surgery tell their patients that they will be back to wearing shoes and back to activity faster than traditional open surgery. This is usually not true as they recovery in a similar amount of time.
4) Next misconception: if your doctor tells you that you’ll be back to normal shoes and normal activity in anything less than three or four weeks when he/she is doing bone surgery (and mostly any other foot surgery), he/she is lying to you. It takes 4 to 6 weeks for bones to heal and be strong after they are cut during surgery (or when they are fractured in an injury). After bone surgery, the patient should be immobilized in a boot or a surgical shoe for this 4 to 6 week period in order to allow the bones to heal properly. Occasionally, people wear a brace for only 3 weeks, but that is more unusual, as almost all of my patients wear it for 4 weeks. Whenever bones are cut, and with any other surgeries, there will be scar tissue that forms in the operative site. The doctor will call this “induration”. This induration will be present for 3-6 months and many times up to a year. During this time, the surgical site will feel hard and stiff. Your doctor may prescribe physical therapy after surgery to break up some of these adhesions. All surgeries produce this scar tissue. It does not mean that you will not be able to perform activities or not wear shoes, but I tell my patients that this will be present and they will not be able to wear all shoes or perform all activities due to it.
5) The last misconception that I hear patients talk about is that foot surgery is extremely painful and even more painful than other types of surgery. The truth is that foot surgery is unique compared to surgery on other parts of the body because you have to walk on your foot postoperatively. This weight bearing and not elevating the part of the body does cause slightly increased pain and throbbing. There are surgical techniques that I employ in order to reduce the amount of pain postoperatively. The amount of pain that patients experience starts with how the surgeon handles the tissue during the surgery. In my residency I was fortunate to work with plastic surgeons that taught me unique tissue handling skills that reduce postoperative pain and swelling. Most of my patients experience moderate to no pain after surgery. While I cannot guarantee that for everyone, I invite potential patients to read my reviews in Google. Many of them state that they had little to no pain, or experience less pain than they expected to have after foot surgery. Additionally, I often prescribe a cold therapy device to be used postoperatively. I also prescribed painkillers that reduce the discomfort after surgery greatly. Most people only take these for 1-3 days after surgery. Having less pain really enhances the surgical experience and lets patients return to more normal activities sooner. For example, most of my patients that have desk jobs are able to go back to work on Monday after doing surgery on Friday.
As you can see, there are many misconceptions about foot surgery. I have generalized my descriptions, however, many variables will affect each individual patient. When patients come in for their preoperative appointment, I am very thorough and go over the following: Alternatives to surgery, risk versus reward of surgery, benefits of surgery, pre-operative planning, postoperative course, potential for further surgery in the future, preventative care against recurrence of the deformity, and any other unique characteristics for the individual patient. I will answer all of your questions and make you feel comfortable about having surgery prior to moving forward with the actual surgery.
To summarize the most important points of this blog: 1) Don’t do minimally invasive surgery. (Yes, it is THAT bad that I can generalize). 2) There are ways to reduce postoperative pain. 3) Have realistic expectations about recovery. 4) There are ways to reduce surgical scarring. 5) There are surgical techniques to make foot surgery more cosmetic while getting rid of painful foot deformities.
The Best Hammertoe Surgeon and Why
In my residency training I was very lucky to have a good friend who was a plastic surgery fellow. (Fellowship comes after residency in a doctor’s training, and is very specialized.) My friend taught me various plastic surgery procedures and tricks that I have applied to my foot surgery.
Hammertoe Surgeon
For example:
When surgeons do hammertoe surgery, part of one of the toe bones is removed in order to straighten out the toe. When the bone is removed, the toe is shortened, which is one of the goals of the procedure in order to reduce the contracture of the hammered toe.
When the bone is shortened, the skin length stays the same. As a result of this, there is bunching up of the skin. As an analogy, picture wearing a knitted glove that is too large for your hand. When you push the glove on to touch the tip of your finger, the excess material will be bunched up and folded.
Most doctors remove the part of the skin directly under the incision in order to shorten it however, they leave the excess skin on the other three sides of the toe and try to just suture it down, but inevitably, there is excess skin left over that will always be there at the edges of the incision. I’ve heard so many doctors in my training and in practice say that the skin just “reabsorbs”. This is not true, but they just don’t know how to fix this problem.
Enter my friend the plastic surgeon… He taught me how to do this complex but tiny procedure called the skin plasty. Through a series of diagonal cuts, triangles, and diamonds, I can reshape the excess skin into a round toe again. This involves using straight incisions at angles to one another that remove the excess skin and create a round toe.
I employ these skin plasty procedures in every surgery I do in order to create a more cosmetic outcome while fixing the foot deformity but in hammertoe surgery they are the most important.
In addition, he taught me a variety of other tricks to get the most cosmetic result while fixing the underlying orthopedic problem and relieving foot pain like just a few that I have listed below:
- The first technique is simply incision planning. Where you place in incision is very important and differs from patient to patient.
- The technique of suturing makes a huge difference in the appearance of scars. Both the skin suturing and the suture closure of deeper layers.
- Tissue handling techniques makes a big difference in reducing postoperative pain and reducing postoperative swelling. This includes which instruments the doctor uses during the surgery.
- Bandaging techniques even make a small difference.
My friend allowed me to scrub cases with him doing breast augmentations, tummy tucks, face lifts and many other plastic surgery procedures. I think of him every Friday when I perform foot surgery, and am thankful that he taught me how to be a better surgeon.
Below are before and after pictures of hammertoe surgery (click any picture to make larger):
BELOW: Pre-operative photo of foot with third digit hammertoe and corn.
BELOW: Post-operative photo of hammertoe surgery at five days.
BELOW: Post-operative photo of hammertoe surgery at only four months.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42ns St, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.What are Hammertoes? Prevention and Hammertoe Surgery.
Allow me to share some information in layman’s terms on hammertoes and Hammertoe surgery. The four small toes on the foot are similar in composition to the fingers. Each of the small toes has three bones with joints in between. The toes form a joint,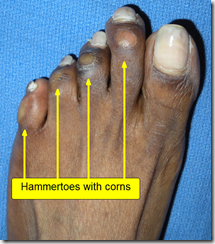 meeting in what is called the ball of the foot. These bones in
meeting in what is called the ball of the foot. These bones in 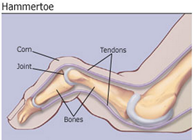 the small toes are normally straight, but when they become bent (at the first joint), it results in hammertoe. Hammertoe can occur in any of these small toes. Usually, the bend also causes a growth similar to a deep blister, called a bursa. This bursa can become inflamed and eventually, hard callusing and corns can occur.
the small toes are normally straight, but when they become bent (at the first joint), it results in hammertoe. Hammertoe can occur in any of these small toes. Usually, the bend also causes a growth similar to a deep blister, called a bursa. This bursa can become inflamed and eventually, hard callusing and corns can occur.
At the beginning of the deformity, the toe can be straightened. With time, however, the joints become rigid. This can then affect the joint at the ball of the foot and, sometimes causing the joint capsule to tear. The joint is then dislocated and the toe points upward. Painful hammertoes require attention before the condition worsens.
What are the causes of hammertoe?
- Improper footwear, especially in women who wear high heels or ill-fitting shoes

- Improper function of the foot itself during walking
- Trauma or injury to the foot either from a direct blow or overuse
- Diabetes or rheumatoid arthritis can predispose a person to hammertoe
What are the some symptoms of hammertoe?
- Prominence or deformity of a toe accompanied by pain
- Redness around the painful joints
- Swelling around the afflicted joints
- Corns on toes
- Calluses on toes
- Difficulty wearing shoes, from painful toes which may also be deformed
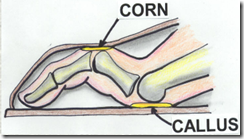
- Difficulty walking
- Stiffness in the toe joints
An examination by a qualified podiatrist, a medical history and X-rays to determine the extent of the damage and arthritis in the joint are usually required to make the proper diagnosis. Simply having ugly toes isn’t a reason to naturally assume that you have hammertoe unless the “ugliness” is accompanied by the symptoms listed above.
Is there anything you can do to help alleviate the pain?
- You can wear proper fitting shoes with a large toe area
- You should avoid wearing high heels
- You can wear a protective pad over the toe(s) that cause the problem
- You can visit a qualified podiatrist for an assessment and
 treatment. The podiatrist can
treatment. The podiatrist can  recommend the proper footwear, suggest some exercises if you can still move your toes, teach you how to strap your toe in the correct position, supply you with a splint or padding, assess whether you should consider wearing orthotics or advise you whether you should have surgery.
recommend the proper footwear, suggest some exercises if you can still move your toes, teach you how to strap your toe in the correct position, supply you with a splint or padding, assess whether you should consider wearing orthotics or advise you whether you should have surgery.
Without proper treatment, the hammertoe deformity will become worse and eventually the afflicted toe(s) will become completely stiff and cause severe problems with footwear. Because of the toes being displaced, the ball of the foot will get undue stress, building up corns and calluses, causing a great deal of pain. So, you may be asking yourself what you can do if you begin to develop hammertoe. In the short-term, you can do things to alleviate the pain and discomfort, but in the long-run the only way to rectify the situation is with hammertoe surgery.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.
Keep your foot dry after surgery!
After foot surgery it is important to keep your foot dry. Depending on the procedure it is usually between two and four weeks.
As a convenience for my patients, I dispense a device to keep the foot dry. It works very well in the shower. (click picture to enlarge)
Today, a patient came in and showed me a new use for the shower bag! We received over a foot snow in New York City this week. In order to keep her foot dry after surgery she used her shower bag with her fracture brace to come in for her post-operative appointment.
I thought this was a great idea and thought I would share it. See the pictures below.
cross-posted at: Best Foot Surgeon NYC
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Case Study: severe bunion surgery opening base wedge osteotomy
I am going to start posting quick case studies of interesting foot surgery and other foot problems as they come in. These posts will be shorter than my more education posts and just present the complaint, physical findings, diagnosis and treatment.
The first case study is a severe bunion. This is one of the largest bunions I’ve operated on in my ten years of practice (since 2000).
This patient had severe pain in both of her feet with bunions. The right bunion was bad but the left bunion was really severe.
Here are preoperative pictures. (Click any picture make larger.)
You can clearly see the great toe is under the second toe and how large her bunion is.
Below are the pre-operative x-rays:
You can clearly see the large bunion with the first metatarsal severely angulated.
I decided to do an opening base wedge osteotomy (inserting bone graft to move the metatarsal) . Her first metatarsal was a bit short and if I had done a closing osteotomy (taking out bone to move the metatarsal) it would have shortened it even more, so I didn’t do the closing wedge surgery. After I did the base wedge osteotomy I released the soft tissue contractures at the great toe joint. Then I removed the bump of bone at the first metatarsal joint. Then I did an Akin osteotomy in the toe bone because the first toe was still turned toward the second toe. Then I corrected for the extra skin after moving the bones. After all of these procedures the correction was amazing. There was a new foot! See below.
I called the patient the night of surgery and again the next day and she reported that she had little to no pain even with all the work that I did!
I did surgery two days ago so I don’t have and long term postoperative pictures yet but I did have one of the OR nurses take a picture while still on the operating table at the end of the surgery. I also have immediate postoperative fluoroscopy pictures.
Below are the before and after pictures of this bunion surgery: I will add more long term pictures in the future.
Come back in the future to see pictures of the healing process. I will update below…
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Bunion Surgery NYC – Video that explains bunion surgery in layman’s terms.
Hi again, I’ve been busy working on two blog posts. One is now done and one is almost done. Today I will post one of them:
I’m proud of this project. Below is a link (click on the picture) to a video I made that cleverly explains bunion surgery in layman’s terms. I took part of my usual bunion pain consultation dialog that I have with my patients every day and made a video explaining bunion surgery.
I figure, by making a video about bunion surgery it will be much less dry than reading all about bunion surgery. With that said, the other post I’m working on is a written description of bunion surgery including before and after pictures.
So, click the picture below and enjoy a virtual preoperative consultation on bunion pain and bunion surgery including alternative, conservative choices for bunion pain. Get the popcorn for a riveting eight minutes…
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Congenital duplication of digit, webbed toes, Six toes or four toes, you decide
I had a very nice young lady come in with a complaint of bunion pain.
Webbed Toes
The interesting part of this case though, is not the bunion but a congenital abnormality she had. She had webbing of her second and third toe with duplication of parts of the second toe. What does this mean? I think the pictures will explain it much better than words, see below: (click any picture to enlarge)
Above, you can see the bunion and the congenital abnormality. There are two nails on the second digit and webbing of the skin between the second and third digit. When you see two separate nails you can assume there is duplication of the distal bones as well because the nails are attached to the distal phalanx bones.
In the above x-ray you can see the normal bones of the third toe with three bones, the proximal phalanx, middle phalanx and distal phalanx. You can see the bunion. You can see the two distal phalanx bones and the middle phalanx have all fused into one large bone of the second digit.
Having extra toes (or fingers) is called polydactyl. It is a congenital anomaly and can be hereditary (runs in families) but not always. Treatment depends on the presentation and is usually optional. If there are concerns from the parents of future disability or shoe fitting problems surgery is often performed as an infant. Surgery also depends on which toe is duplicated. In the above patient, surgery would rarely be performed due to difficulties making the toes look normal. The nails are virtually impossible to combine. I’ve done surgery to remove the webbing of the toes using skin flaps and skin grafts. Surgery is much more often performed when there is duplication of the first or fifth digit which tend to make fitting shoes difficult and have an excellent cosmetic prognosis.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Foot Trauma, fracture of the interphalangeal joint of the great toe:
Today I’d like to tell you about a foot trauma case. A young lady presented to my office with a chief complaint of pain in her right great toe. She stated that two days prior she fell off her bicycle. She said the pain was not terrible however when she looked at her foot her great toe was bent at 90° at the joint in a direction where it usually does not go. She quickly grabbed the toe and popped it back into place. She then had increased pain. She says that the toe swelled up immediately after her fall.
Physical examination revealed an extremely swollen and bruised right great toe with severe pain to palpation. I checked to make sure there was good blood flow by pressing on the distal aspect of the toe and noted that the color blanched and came back within 3 seconds. She also had normal feeling in the tip of the toe indicating that there was no nerve injury.
Her x-ray (seen below) showed a mildly displaced fracture of the distal phalanx of the great toe. She did an excellent job at putting the toe back into position from the dislocated joint. This joint, is called the interphalangeal joint. (Intra-articular, mildy displaced fracture of distal phalanx of hallux) (click and any picture to enlarge)
Treatment: I immobilized her in a fracture brace that she will wear for 4-6 weeks. Had she not reduced the dislocation I would have given her local anesthesia and popped it back into place in my office. I advised her that since the fracture enters the joint that she may experience osteoarthritis in this joint at some time in the future.
When a fracture enters the joint it disrupts the cartilage on the end of the bone. When you having injury to the cartilage over time it may wear away and cause arthritis such that the two bones grind together. If this is the case, she will most likely require surgical intervention. In that case what I do is remove the cartilage completely from both bones and fuse the joint with a screw. When the two bones heal they become one bone. When people have arthritis joint fusions are very often used to alleviate the pain. In theory, if there is no motion at the joint then there is no pain at the joint.
The below picture is not of this patient, however, this is what a joint fusion (arthrodesis) with headless screw of the interphalangeal joint looks like:
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Painful Tailor’s bunion, surgical correction of Tailor’s bunion.
Tailor’s Bunion Surgery
Today a young lady came in with a complaint of a large bump behind her fifth toe and added that her fifth toe is turning under her fourth. She has pain when she runs and works out. This has been getting progressively worse over the past six months.
I diagnosed her with a Tailor’s Bunion (also called a Bunionette). See picture below: (click any picture to enlarge)
Tailor’s bunion is a prominence of the fifth metatarsal bone at the base of the little toe. The deformity received its name because tailors sat cross-legged all day with the outside edge of their feet rubbing on the ground. This constant rubbing led to a painful bump at the base of the little toe.
Usually a tailor’s bunion is caused by an inherited faulty mechanical structure of the foot. In these cases, changes occur in the foot’s bony framework, resulting in the development of an enlargement. The fifth metatarsal bone starts to protrude outward, while the little toe moves inward. This shift creates a bump on the outside of the foot that becomes irritated whenever a shoe presses against it. Sometimes a tailor’s bunion is actually a bony spur (an outgrowth of bone) on the side of the fifth metatarsal head.
In the case of this patient, the fifth metatarsal bone was angulated toward the outside.
Treatment for tailor’s bunion: I informed her all about the surgical correction of Tailor’s Bunion where I make a small incision On the side of the foot and access the bone. I then cut a small wedge in the bone to change the angle toward the inside of the foot. After the bone wedge is removed, I placed a tiny titanium screw in order to hold it in place to heal.
Recovery from tailor’s bunion surgery: For people with a desk job I can do the surgery on a Friday and send them back to work on Monday in a surgical shoe or boot. This patient, however, has a job in which she is on her feet doing sales. I advised her that she would need to take 2-3 weeks off of work or work at a desk if possible. She chose to wait until the Fall to perform her surgery when her work schedule is lighter and she can work in the office, rather than on her feet doing sales calls.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Another soft tissue mass to remove this week. – podiatrist NYC
In May I removed a soft tissue mass from this patients left big toe. The pathology report came back as “epidermal inclusion cyst”. In layman’s terms this occurs when the outside dead layer of skin, the epidermis is inverted into the live dermal layer deeper where it does not belong.
Well, after removing the lesion I thought it was all gone, but the patient came back with a recurrence.
Today I had her come back and I excised the lesion and sutured her up. I’m pretty confident that the lesion is now gone forever… (click any picture to enlarge)
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Recurrent Ganglion of tendon sheath – Podiatrist NYC
I just saw a patient with a recurrent ganglion of tendon sheath.
She had presented to my office with a large fluid filled mass on top of her right great toe that had been present for three months and was getting larger. She reported that it rubbed on her shoes and caused pain.
Twice previously I aspirated (sucked out with a needle and syringe) clear gelatinous material from this large ganglion and injected steroid (Kenalog, like cortisone) into the lesion and now twice it has returned. I scheduled her for surgical excision of the ganglion tomorrow in my office under local anesthesia. I will make an incision, cut it out and put in stitches.
I didn’t get a clinical photo, but here’s her ultrasound of the ganglion. It shows up as a large black (hypo-echoic area). Ultrasound bounces sound waves off of things. When it hits bone it makes nice white lines. Soft tissues show up as different shades of gray depending on their density and fluid shows up as black because it doesn’t bounce sound waves off, they go right through the fluid. (click any picture to enlarge
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Severe ingrown toe nail “paranychia” – Podiatrist NYC
It’s only 8:30 AM and this morning I have already performed a small nail surgery. The young man in the photo below had an ingrown nail for 3 weeks but could not make it in to see me because of his work schedule. He finally called in sick and came in with an extreme pain in his right big toe. (click any picture to enlarge)
Treatment: I performed a local anesthesia block with 1% lidocaine. This entails two injections to get all four major nerves of the big toe. Then, I removed the medial (inside) border of the nail. I prescribed antibiotics to be take twice daily for five days. He will follow up in one week.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Unusual toe infection – Podiatrist NYC
I had a young lady come in this morning with a complaint of pain on the bottom of her right second toe for 4 days. She reported a small callus on the bottom of the toe that had just started and was painful when running.
Physical exam revealed a 2x3mm callus. It looked like this:
I debrided (scraped) the callus and was surprised to find a 3mm hair in there surrounded by a small amount of pus.
She owns a hair salon and works in flip-flops sometimes. A small piece of human hair had entered a pore in her toe and caused an infection.
I removed the hair, drained the pus and applied topical Gentamicin antibiotic cream. She’s going to live…
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Case of the day – fibular stress fracture – Podiatrist NYC
For my first patient post allow me to tell you about a patient that came in yesterday:
A 29-year-old female came in with the complaint of swelling and pain in her left ankle. She states that she had been running for eight days straight and on the eighth day she experienced significant pain and swelling of her ankle during and after her run. She indicated the area outside of her ankle at and just above her ankle joint.
Physical examination revealed that she had pain with pressure on the outside of her ankle. There was significant swelling. There was pain with range of motion. There was pain at the ankle ligaments that appeared to be an ankle sprain. However, she reported that she never twisted or injured her ankle.
X-Ray examination revealed what looked like a stress fracture of the fibular bone. See x-ray below: (click any picture to enlarge.)
Fibular Stress Fracture
This is how I explain what a stress fracture is to my patients, “A stress fracture is not like a regular fracture. To give you an analogy, a regular fracture is like a pencil. You apply force once and break it in half. A stress fracture is more like a paper clip. You apply force over and over again to bend it. It breaks on the inside before it breaks all the way through. If you continue to apply force to bend it, it eventually it breaks all the way through.”
Stress fractures don’t always show up on x-ray like above. Just like the paperclip analogy, you could not tell that the paperclip is broken by looking at it before it breaks all the way through.
Treatment for the stress fracture is immobilization in a fracture brace for four to six weeks. Prior to putting a patient in a fracture brace I often like to confirm the presence of a stress fracture with an MRI if there is any question on the x-ray. I don’t like to torture patients by making them wear the brace for four weeks if I’m not sure it is a stress fracture.
The above patient will likely wear her brace for four to six weeks and then slowly increase her activity and run again in six to eight weeks.
Note: in my ten years of practice, I’ve never had a patient come back with a stress fracture in the same bone twice. They’ve come back with other bones with stress fracture, but never the same bone.
© Copyright 2010 Best Podiatrist NYC Emanuel Sergi, DPM City Footcare, PC 122 E 42nd Street, Ste 2901 New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.Welcome to the City Footcare Podiatry Blog
Greetings! I started this blog to talk about foot problems.
As a podiatrist in New York City (NYC) I get to see so many diverse foot problems. The name of the blog came from my Google Analytics. The most searched term to find me on Google has been “Best Podiatrist NYC”. So, as a humble person, I cannot take credit for the title completely.
What I would like to do is present actual cases of my patients that come in. (Names withheld of course.) Every day I see the usual common problems like plantar fasciitis (heel pain), neuromas (nerve pain), ingrown toe nails, nail fungus (onychomycosis), tendonitis, joint pain, fractures, bunions, hammertoes, arthritis, joint dislocations, soft tissue injuries, tendon tears, ligament tears (strains and sprains), and many other common foot problems. Additionally, everyday more obscure pathologies come in that challenge my diagnostic abilities. I do x-rays, ultrasounds, fluoroscopy and MRI’s.
Every Friday I do foot surgery. This is the most rewarding part of my job. Here, I get to use my mechanical ability to go in there and fix things. Prior to going to medical school I did carpentry work in order to pay for University. I am really good with my hands and tools. I am able to think analytically and visualize the anatomy in three dimensions. I love to modify and refine old procedures as they apply to each individual’s unique pathology in my surgeries. I like to think that my surgical abilities are truly a gift and I love to teach my residents to be better surgeons. My residents love working with me and learning things that other podiatrists don’t teach them.
Going forward I will try to write a little bit here and there and talk about podiatry and anything else that comes to mind. Being my first post I doubt many people will see this, but hopefully I’ll build a following. Please feel free to email me and comment. I will write back.
Thanks for reading,
© Copyright 2010 Best Podiatrist NYC City Footcare, PC 122 E 42nd Street, Ste 2901, New York, NY 10168 212-871-0800 www.cityfootcare.com cityfootcare@gmail.com Specializing in foot surgery, bunion surgery, hammertoe surgery, cosmetic foot surgery, general podiatric surgery.